Pharmacotherapy of Alcohol Dependence
- 3rd leading cause of preventable deaths worldwide à 3 million deaths (5.3% of all deaths) worldwide
- Alcohol intake– Prevalence in India à both in rural and urban – male -23% – 74%, females – 24% to 48 %
Alcohol use disorder –
a cluster of physical and behavioral symptoms which can induce withdrawal, tolerance or craving (DSM V)
- DSM–5 integrates the two DSM–IV disorders, alcohol abuse, and alcohol dependence, into a single disorder called alcohol use disorder (AUD)
- Under DSM–5, anyone meeting any 2 of the 11 criteria during the same 12-month period would receive a diagnosis of AUD
- Eliminates legal problems as a criterion
- Adds craving as a criterion for an AUD diagnosis (Wanted a drink so badly you couldn’t think of anything else?)
- Total of 11 criteria
- Loss of control – 4 criteria
- Impairment – 3 criteria
- Risky/ dangerous use – 2 criteria
- Physiologic – 2 criteria
- Severity based on a number of criteria
- mild – 2-3
- moderate – 4-5
- severe – >6
Metabolism of alcohol
- Absorption – 10% from stomach, 90% small intestine(proximal)
- Peak blood concentration – in 30-90 min
- Metabolism – 80% in the liver (by ADH & ALDH enzymes)
Genetic variation
- ADH1B*2 & ADH1B*3 is protective with a lower risk of AUD & related problems
- Polymorphism in ALDH2 – low levels of acetaldehyde are rewarding & stimulating for alcohol consumption
- Children of alcoholics are at 2-4 folds higher risk
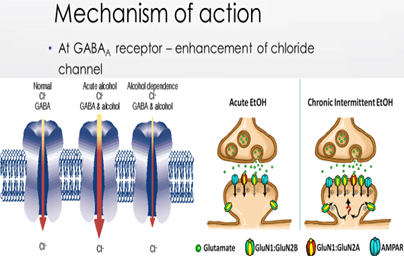
At GABAA receptor – enhancement of chloride channel
Acute administration – increase GABA release inhibit postsynaptic NMDA receptor
Chronic drinking – upregulation of NMDA receptor
Withdrawal – decrease GABA & enhance NMDA activity
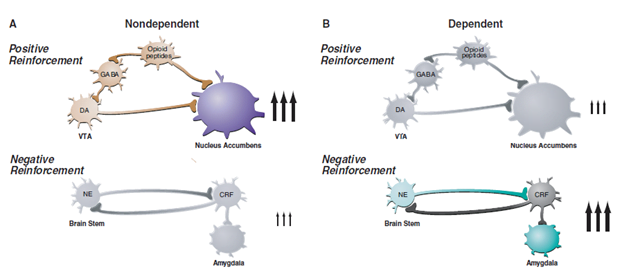
- Alcohol has both positive & negative reinforcing actions in the brain.
- Intake of alcohol increases GABAergic transmission, the release of endogenous opioids & decrease glutaminergic activity à causes the release of DA à in mesolimbic pathway i.e reward center, here person drink to satisfy reward center i.e positive reinforcement.
- But when the patient becomes dependent positive reinforcing effects of alcohol shift to negative reinforcing effects which results from progressive recruitment of the CRH system or STRESS circuit. Here a person’s drinking because of reward craving & here for relief craving.
Withdrawal & Tolerance
Withdrawal – a group of symptoms and signs occurring on cessation or reduction of the use of a psychoactive substance taken repeatedly, for a prolonged period and/ or in high doses
Tolerance –Same amount of substance insufficient, Greater amount to achieve the previous effect
Symptoms
- Tremor of the hands (shakes)
- agitation and anxiety
- autonomic nervous system overactivity including an increase in pulse, respiratory rate, sweating and body temperature
- insomnia.
- Screening
- CAGE QuestionnaireAUDIT Questionnaire
- History taking
- Laboratory diagnosis
CAGE Questionnaire
Consist of 4 questions-
- Have you ever felt to Cut down on your drinking?
- Have people Annoyed you by criticizing your drinking?
- Have you ever felt Guilty about your drinking?
- Have you ever had a morning drink (Eye-opener) to get rid of a hangover?
> 2 or more yes = alcohol misuse
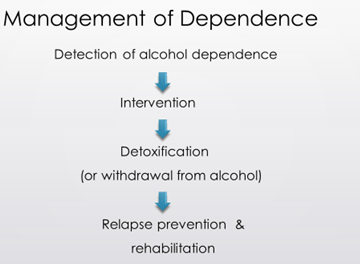
Treatment of chronic alcoholism can be divided into:
- Detoxification: This aims at providing safe withdrawal to make the patient alcohol-free.
- Rehabilitation: which includes (a) Psychotherapy and (b) Institutional therapy.
- Support therapy: to prevent relapses and to assist the patient in maintaining abstinence
- Detoxification:
- If the patient agrees to stop drinking, detoxification is done by withdrawing alcohol.
- perform a thorough physical examination in all alcoholics à evidence of liver failure, gastrointestinal bleeding, cardiac arrhythmia, infection, and glucose or electrolyte imbalance.
- also, important to offer adequate nutrition and oral multiple B vitamins, including 50–100 mg of thiamine daily for a week or more.
- Thiamine – Prevention & treatment of Wernicke’s encephalopathy & Korsakoff’s psychosis
- Magnesium supplement – Mg is needed for normal utilization of Thiamine also, in severe case deficiency is 1-2 mEq/kg body wt.
- Because most alcoholics who enter withdrawal are either normally hydrated or mildly overhydrated, IV fluids should be avoided unless there is a relevant medical problem or significant recent bleeding, vomiting, or diarrhea.
- Glucose is administered IV if there is hypoglycemia.
Because alcohol withdrawal symptoms reflect the rapid removal of a CNS depressant (anxiety, insomnia, agitation) they can be controlled by administering any depressant in doses that decrease the agitation and then gradually tapering the dose over 3–5 days.
benzodiazepines (those with longer half-lives 25–50 mg of chlordiazepoxide or 10 mg of diazepam given orally every 4–6 h on the first day, with doses then decreased to zero over the next 5 days) à have the highest margin of safety and lowest cost and are, therefore, the preferred class of drugs. Though other symptoms respond within 3-5 days, it may take several months to restore normal sleep patterns.
Short-half-life benzodiazepines (oxazepam) can be considered for patients with serious liver impairment or evidence of brain damage, but they must be given every 4 h to avoid abrupt blood-level fluctuations that may increase the risk for seizures.
Carbamazepine, an antiepileptic drug is an effective alternative to benzodiazepines in treating mild to moderate withdrawal symptoms. It prevents seizures and does not cause respiratory depression nor impairs memory. It is relatively safe.
Some patients may experience delirium tremens, where the withdrawal includes delirium (mental confusion, agitation, and fluctuating levels of consciousness) associated with a tremor and autonomic overactivity. à Benzodiazepines in high doses are recommended for this condition as they decrease agitation and raise the seizure threshold but probably do little to improve the confusion.
The use of antipsychotic medications, such as haloperidol or olanzapine, is considered.
Alpha-adrenergic agonist Clonidine 0.1-0.4 mg QID, or beta-blocker Atenolol (orally)50 -100 mg daily may be given to combat autonomic hyperactivity.
- Rehabilitation: include
- use of various cognitive-behavioral approaches,
- counseling,
- vocational rehabilitation, and
- reinforcement through self-help groups such as Alcoholics Anonymous.
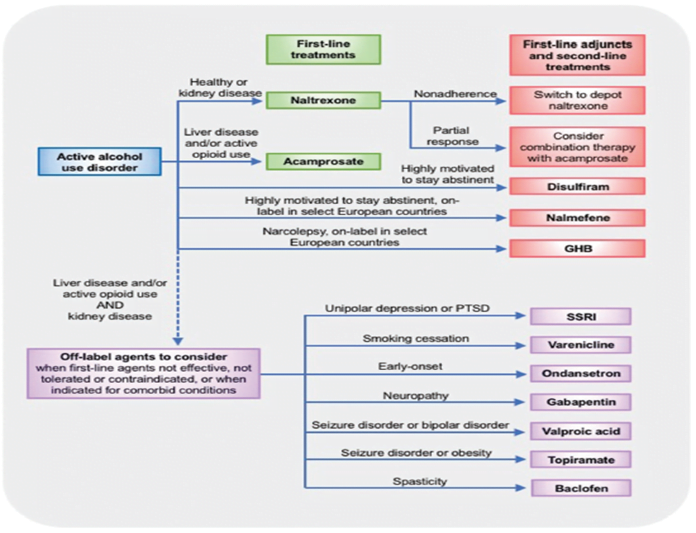
- Support therapy: The following group of drugs can be used to maintain abstinence:
- Opioid antagonists, e.g., Naltrexone, Extended-release, injectable naltrexone, Nalmefene (off label)
- NMDA receptor antagonist, e.g. Acamprosate
- Aversion drugs, e.g., Disulfiram
- Supporting drugs, e.g., Lithium, Carbamazepine, Topiramate
I. The rationale for the use of Naltrexone:
- It is a long-acting opioid antagonist. By blocking opioid receptors, it decreases the activity of these dopaminergic pathways and decrease the feeling of pleasure or reward if alcohol is imbibed. It reduces the intake & desire to take alcohol.
- Naltrexone reduces the craving for alcohol. The number of drinking days & chances of resumed heavy drinking are also reduced.
- The most common side effect of naltrexone is nausea. When given in excessive doses, naltrexone can cause liver damage. It is contraindicated in patients with liver failure or acute hepatitis.
- Start with 25 mg/day
- Maintenance-50 mg/day
- S/E – Somnolence (29.5%), nausea, vomiting, decreased appetite, abdominal pain, insomnia, dizziness
Extended-release Naltrexone
- Patients able to abstain from alcohol in an outpatient setting
- FDA approved – 2006 at a dose of 380 mg/month i.m.
- Adverse events as oral naltrexone and also injection site reactions
II. The rationale for use of Acamprosate (N-acetyl homotaurine):
- Acamprosate acts possibly by blocking the NMDA subtypes of ionotropic glutamate receptors and activating GABA-A receptor in the brain.
- It decreases the frequency of drinking without affecting the food or water intake & decreases relapse drinking in abstinent alcoholics.
- It reduces relapse both short term & long term especially when used with psychotherapy.
- The effectiveness of acamprosate is increased when used with disulfiram without any adverse interaction.
- Acamprosate tablets: 333 mg, recommended dose for adults >60kg being 1998mg (six tablets/day, orally in three doses: 2; 2; 2).
- Before a meal (as food interferes with absorption)
- s/e Most common: gastrointestinal adverse effects: diarrhea, resolving spontaneously
- Mild abdominal pain, rash, paresthesia, altered libido and confusion reported at low frequencies
- Treatment period: 3-6 months.
- The decision should be made on a case-by-case basis.
Suitability for Acamprosate
- Compliant & stable patients with alcohol dependence (usually, moderate to severe)
- More effective for patients with an abstinence goal
- Safety of acamprosate in pregnancy or lactation NOT established
III. The rationale for the use of aversion therapy:
Usually, alcohol consumption produces a pleasant feeling- feeling of well-being. Disulfiram is used to make alcohol consumption an unpleasant experience so that the person gives up drinking. This happens because:
- Disulfiram inhibits enzyme acetaldehyde dehydrogenase which handles the metabolism of ethanol.
- Thus, on alcohol consumption, accumulation of acetaldehyde occurs, which can produce flushing, throbbing headache, nausea, vomiting, sweating, thirst, hypotension, chest pain, confusion (Antabuse reaction).
- The effect persists for 2 weeks after the last dose of disulfiram as 2 weeks’ time is required for the restoration of enzymatic activity.
- As Antabuse reaction can be dangerous, especially for patients with heart disease, stroke, diabetes mellitus, or hypertension, the treatment should be preferably given in a hospital under strict medical supervision.
- The drug itself carries potential risks of depression, psychotic symptoms, peripheral neuropathy, and liver damage. Disulfiram should be administered to the patient who is motivated and willing to give up drinking.
- Disulfiram has a long history of use but has fallen into disfavor because of its side effects and problems with patient adherence to therapy
- Before starting disulfiram, pt. should be abstinent from alcohol for 12 hours
- Dose – 125-500mg OD
IV. Other Supporting drugs:
- Lithium: It acts as a mood stabilizer and reduces alcohol consumption.
- Ondansetron: It is a 5-HT3 antagonist. It is effective in early-onset alcoholics in whom the response to psychosocial treatment is poor. It lowers the amount of alcohol consumed & the subjective effects of alcohol are also reduced.
- Topiramate: An anti-epileptic drug. It reduces the craving for alcohol & increases the abstinent days. Its mechanism of action is unclear.
A combination of 2 or more treatment modalities is useful rather than using a single drug.