Anti-platelet agents
- interfere with platelet function and are useful in the prophylaxis of thromboembolic disorders
- In veins, due to sluggish blood flow, a fibrinous tail is formed which traps RDCs ‘ the red tail ‘.
- In arteries, platelet mass is the main constituent of the thrombus.
- Antiplatelet drugs are, therefore, more useful in arterial thrombosis. while anticoagulants are more effective in venous thrombosis.
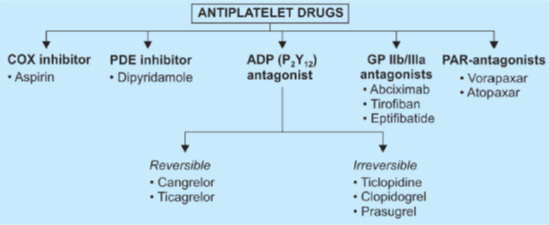
COX inhibitor à Aspirin
- acetylates the enzyme COX I and TX-synthase- inactivating them irreversibly. TXA2 activates platelets to change shape and release mediator rich granules that promote aggregation.
- Because platelets cannot synthesize fresh enzyme (have no nuclei), TXA2 formation is suppressed at very low doses and till fresh platelets are formed. Thus, aspirin-induced prolongation of bleeding time last for 5- 7 days
- Maximal inhibition of platelet function occurs at 75- 150 mg aspirin per day.
- (ACC/AHA)* guidelines recommend a dose of 75- 162 mg/ day for long-term aspirin prophylaxis.
- higher doses (> 900 mg/day) may decrease both TXA2 and PGl2 production
- PGI2 is strong inhibitor of platelet aggregation, therefore low doses used.
- Other NSAIDs arc reversible inhibitors of COX, produce shor1-las1ing inhibition of platelet function-are not clinically useful.
PDE inhibitor à Dipyridamole
- inhibits phosphodiesterase as well as blocks uptake of adenosine to increase platelet cAMP which in turn potentiates PGI2 and interferes with aggregation
- Dipyridamole alone has a little clinically significant effect. but improves the response to warfarin, along with which it is used to decrease the incidence of thromboembolism in patients with prosthetic heart valves.
- Dipyridamole has also been used to enhance the antiplatelet action of aspirin. This combination may additionally lower the risk of stroke in patients with transient ischemic attacks (TIAs)
ADP antagonist
- Ticlopidine à acts by blocking the P2Y 12 receptors on the surface of platelets and inhibits ADP-induced aggregation.
- s/e- neutropenia and thrombocytopenia
- Clopidogrel à more potent congener of ticlopidine, the same range of therapeutic efficacy, but is safer and better tolerated (CLASSICS study).
- A combination of clopidogrel and aspirin is synergistic in preventing ischemic episodes à ‘ dual antiplatelet therapy’ (DAPT) is also utilized for checking restenosis of stented coronaries. à but increase bleeding risk
- Omeprazole, an inhibitor of CYP2C 19, reduces metabolic activation of clopidogrel and its antiplatelet action.
- The action lasts for 5 days due to the irreversible blockade of platelet P2Y 12 receptor.
- The most important adverse effect is bleeding
- Prasugrel à newer most potent and faster-acting P2Y12 receptor blocker.
- interference by omeprazole treatment has not been prominent.
- Because of rapid action, prasugrel is particularly suitable for use in STEMI.
- Preferred thienopyridine in ACS to cover angioplasty with or without stent placement.
- Superior clinical outcomes and reduction in Stent thrombosis have been obtained with prasugrel.
- Ticagrelor à latest P2Y12 receptor inhibitor –ORAL
- acts directly without needing metabolic activation.
- Unlike clopidogrel and prasugrel, the action of ticagrelor is reversible. Thus, it has a faster onset and quicker offset of action; the biological t½ is 12 hours, and it needs twice-daily administration
- The PLATO trial compared ticagrelor with clopidogrel in patients with ACS and reported lower cardiovascular mortality as well as all-cause mortality with ticagrelor.
- The risk of intracranial bleeding was higher with ticagrelor, but that of all major bleeds was similar
- The European guidelines now recommend that all patients at high risk of ACS be given prophylactic ticagrelor
- Cangrelor à intravenous
- Vorapaxar, Atopaxar à PAR antagonist
- Orally active inhibitor of thrombin receptors on platelet called protease-activated receptor 1
- Approved as an antiplatelet drug in patients with a history of MI or peripheral artery disease.
Glycoprotein (GP) IIb/ Illa receptor antagonists
- GP IIb/ IIIa is an adhesive receptor (integrin) on platelet surface for fibrinogen and vWF through which agonists like collagen, thrombin, TXA2, ADP, etc. finally induce platelet aggregation.
- Thus, GP IIb/ IIIa antagonists block aggregation induced by all platelet agonists.
- used only in patients with ACS and to cover PCT or coronary artery bypass grafting (CABG).
- Abciximab àa chimeric monoclonal antibody against GP IIb/ IIIa protein
- S/e à hemorrhage, thrombocytopenia
- It is expensive. but is being used in unstable angina and as an adjuvant to coronary thrombolysis/ PCI with stent placement
- Eptifibatide
- Tirofiban
Uses of antiplatelet drugs
- To prevent intravascular thrombosis and embolization, with minimal risk of hemorrhage.
- Those with CAD or risk factors for stroke are generally given a single drug (aspirin/ clopidogrel).
- For indications like ACS, maintenance of vascular recanalization, stent placement, vessel grafting, etc. potent inhibition required à (dual antiplatelet therapy).
- Coronary artery disease
- it is recommended that aspirin 75- 150 mg/day be given to all individuals with evidence of coronary artery disease
- It reduces the incidence of fatal as well as nonfatal MI but increases the risk of a cerebral hemorrhage.
- Continued aspirin/ clopidogrel prophylaxis in post-Ml patients clearly prevents reinfarction and reduces mortality.
- Acute coronary syndromes (ACS)
- range of acute cardiac ischemia states from unstable angina (UA) to non-ST elevation myocardial infarction (NSTEMI) to STEMI
- Soluble aspirin (325 mg oral) and an LMW heparin (s.c.) are given at presentation to all patients with ACS.
- Unstable angina à Aspirin reduces the risk of progression to MI and sudden death.
- Clopidogrel is generally combined with aspirin or may be used as an alternative if aspirin cannot be given.
- For maximum protection, the antiplatelet drugs are supplemented with heparin followed by warfarin.
- NSTEMIà Patients of NSTEMI who are managed without PCI/thrombolysis are generally put on a combination of aspirin + clopidogrel, which is continued up to one year.
- STEMI à Primary PCI with or without stent placement is the procedure of choice for all STEMI as well as high-risk NSTEMI patients who present within 12 hours.
- Prasugrel + aspirin is the antiplatelet regimen most commonly selected for patients who are to undergo PCI.
- Prasugrel acts rapidly and more predictably than clopidogrel. Prasugrel is also preferred over clopidogrel in diabetics.
- The GPIIb/IIIa antagonists are the most powerful antiplatelet drugs; they are combined with aspirin for high-risk patients undergoing PCI.
- Prasugrel is used when stent thrombosis occurs during clopidogrel treatment.
- Cerebrovascular disease
- aspirin has reduced the incidence of TIAs and stroke in patients with TIAs.
- Prosthetic heart valves and arteriovenous shunts
- Antiplatelet drugs used with warfarin reduce the formation of microthrombi on artificial heart valves and the incidence of embolism.
- Venous thromboembolism
- Anticoagulants are routinely used in DVT and PE.
- Trials have shown antiplatelet drugs also to have a prophylactic effect, but their relative value in comparison to, or in addition to anticoagulants is not established; they are infrequently used.
- Peripheral vascular disease
- Aspirin/clopidogrel may produce some improvement in intermittent claudication and reduce the incidence of thromboembolism.
Current usage
The use of antiplatelet therapy (including ASA, aspirin) for stroke prevention in AF is increasingly limited:
- Although antiplatelet agents reduce the risk of stroke in patients with AF, they are less effective than anticoagulant therapy
- In the AVERROES study, apixaban was superior to ASA for stroke prevention and was associated with a similar rate of major bleeding
Guideline recommendations
Recent guidelines have highlighted the limited risk-benefit of antiplatelet therapy for stroke prevention based on the efficacy profile and potential for causing serious bleeding events:
- American College of Chest Physicians (ACCP) 2012 guidelines limit the recommendation for ASA to an option for patients with AF with a low risk of stroke (although oral anticoagulation is preferred), or patients with AF and no stroke risk factors (with no antithrombotic therapy preferred over ASA therapy)
- ESC 2016 guideline update: Antiplatelet therapy is not recommended for stroke prevention in patients with AF
- In contrast, the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) 2014 guidelines for the management of patients with AF still include ASA as an option for patients with a moderate risk of stroke
2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease
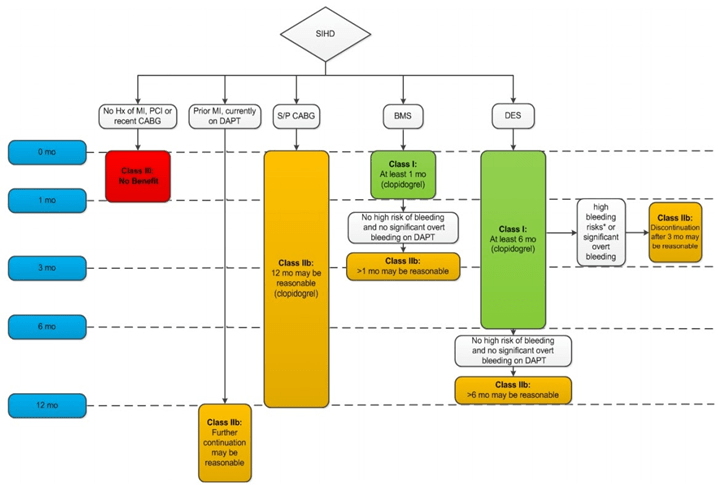
Patients with a history of ACS > 1-year prior who have since remained free of recurrent ACS are considered to have transitioned to SIHD. Arrows at the bottom of the figure denote that the optimal duration of prolonged DAPT is not established. Clopidogrel is the only currently used P2Y12 inhibitor studied in patients with SIHD undergoing PCI. Aspirin therapy is almost always continued indefinitely in patients with coronary artery disease.
*High bleeding risk denotes those who have or develop a high risk of bleeding (e.g., treatment with oral anticoagulant therapy) or are at increased risk of a severe bleeding complication (e.g., major intracranial surgery). ACS indicates acute coronary syndrome; BMS, bare metal stent; CABG, coronary artery bypass graft surgery; DAPT, dual antiplatelet therapy; DES, drug-eluting stent; Hx, history; MI, myocardial infarction; PCI, percutaneous coronary intervention; SIHD, stable ischemic heart disease; and S/P, status post.
