Antidiuretics Hormone (Argenine Vasopressin-AVP)
- inhibit water excretion without affecting salt excretion à drugs that reduce urine volume, particularly in diabetes insipidus (DI) which is their primary indication.
- Drugs are:
1. Antidiuretic hormone (ADH, Vasopressin) à Desmopressin, Lypressin, Terlipressin
2. Thiazide diuretics à Amiloride.
3. Miscellaneous: Indomethacin, Chlorpropamide, Carbamazepine.
The two main hormones released from neurohypophysis (posterior pituitary ) are Oxytocin & ADH
ADH Synthesis à Supraoptic nucleus(SON) – 75% & Paraventricular nuclei (PVHN) -3%
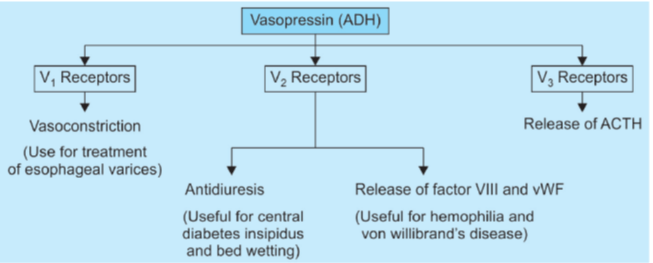
Actions of ADH
- ADH increases the permeability of Collecting duct by its action on V2 receptors. à elevates cAMP levels that increase aquaporins on the apical membrane of CD (by decreasing endocytosis and increasing exocytosis).
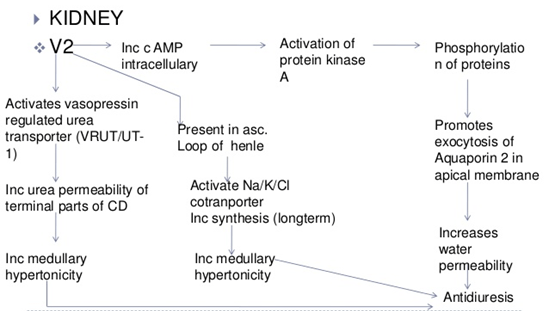
- V2 receptor activation also increases permeability of CD to urea by stimulating the urea transporter.
- Vasopressin (ADH) à a potent pressor of blood vessels à Vasoconstrictor action is mediated by the activation of V1 (also called V1a) receptors.
- ADH is also involved in the release of vWF and factor VIII from the endothelium à mediated by V2 receptors.
- V3 receptors (previously known as V1b receptors) are involved in the release of ACTH.
VASOPRESSIN ANALOGUES
Lypressin
- less potent than AVP
- acts on both V1 and V2 receptors and has longer duration of action (4–6 hours).
- It is being used in place of AVP—mostly for V1 receptor mediated actions.
Terlipressin
- synthetic prodrug of vasopressin
- specifically used for bleeding esophageal varices
Desmopressin (dDAVP)
- synthetic peptide is a selective V2 agonist;
- 12 times more potent antidiuretic than AVP, but has negligible vasoconstrictor activity.
- also longer acting because enzymatic degradation is slow; t½ 1–2 hours; duration of action 8–12 hours.
- preparation of choice for all V2 receptor related indications.
- The intranasal route is preferred, though bioavailability is only 10–20%.
- An oral formulation has been recently marketed with a bioavailability of 1–2%; oral dose is 10–15 times higher than intranasal dose, but systemic effects are produced and nasal side effects are avoided.
Uses
A. Based on V2 actions (Desmopressin is the drug of choice)
1. Diabetes insipidus
Diabetes insipidus is a lack of antidiuretic hormone (ADH) or a lack of response to ADH. This prevents the kidneys from being able to concentrate the urine leading to polyuria (excessive amounts of urine) and polydipsia (excessive thirst). It can be classified as nephrogenic or cranial.
The major symptoms of central diabetes insipidus (DI) are polyuria, nocturia, and polydipsia due to the concentrating defect.
Treatment of this disorder is primarily aimed at decreasing the urine output, usually by increasing the activity of antidiuretic hormone (ADH, also called arginine vasopressin or AVP).
Water Deprivation Test
The water deprivation test is also known as the desmopressin stimulation test. This is the test of choice for diagnosing diabetes insipidus.
Method
Initially the patient should avoid taking in any fluids for 8 hours. This is referred to as fluid deprivation. Then, urine osmolality is measured and synthetic ADH (desmopressin) is administered. 8 hours later urine osmolality is measured again.
| Diagnosis | After Deprivation | After ADH |
| Cranial Diabetes Insipidus | Low | High |
| Nephrogenic Diabetes Insipidus | Low | Low |
- DI of pituitary origin (neurogenic) is the most important indication for vasopressin.
- ineffective in renal (nephrogenic) DI, since kidney is unresponsive to ADH.
- Lifelong therapy is required, except in some cases of head injury or neurosurgery, where DI occurs transiently.
- The dose of desmopressin is individualized by measuring 24 hour urine volume.
- Aqueous vasopressin or lypressin injection is impracticable for long-term treatment.
- It can be used in transient DI and to differentiate neurogenic from nephrogenic DI—urine volume is reduced and its osmolarity increased if DI is due to deficiency of ADH, but not when it is due to unresponsiveness of kidney to ADH.
- Desmopressin 2 μg i.m. is the preparation of choice now for the same purpose.
Other drugs that may decrease diuresis include chlorpropamide, carbamazepine and clofibrate, nonsteroidal anti-inflammatory drug (NSAID) and thiazide diuretics.
2. Bedwetting in children and nocturia in adults
- Intranasal or oral desmopressin at bedtime controls primary nocturia by reducing urine volume.
- Nocturnal voids are reduced to nearly half and first sleep period in adults is increased by ~2 hr.
- Fluid intake must be restricted 1 hr before and till 8 hr after the dose to avoid fluid retention.
- Monitor BP and body weight periodically to check fluid overload.
- Withdraw for one week every 3 months for reassessment.
3. Renal concentration test
- 5–10 U i.m. of aqueous vasopressin or 2 μg of desmopressin causes maximum urinary concentration.
4. Haemophilia, von Willebrand’s disease
- may check bleeding by releasing coagulation factor VIII and von Willebrand’s factor.
- Desmopressin is the preferred preparation in a dose of 0.3 μg/kg diluted in 50 ml saline and infused i.v. over 30 min.
- DDAVP should only be used for mild bleeding for which a 30- to 60-minute delay is acceptable (for elective procedures in patients with mild hemophilia A) and a two- to fourfold factor VIII increase are likely to be sufficient for hemostasis. For more serious bleeding, factor VIII infusion should be used.
B. Based on V1 actions
1. Bleeding esophageal varices
- Vasopressin/terlipressin often stop bleeding by constricting mesenteric blood vessels and reducing blood flow through the liver to the varices, allowing clot formation.
- Terlipressin stops bleeding in ~80% and has been shown to improve survival. (only agent individually shown to reduce mortality)
- Pharmacologic therapy should be started at the time of presentation in a patient who has known varices or is at risk for varices. It should not be held pending confirmation of the diagnosis. Terlipressin is the preferred agent in many countries. It is initially given as 2 mg intravenous (IV) bolus every four hours.
- It has replaced AVP because of fewer adverse effects and greater convenience in use.
- Octreotide (a somatostatin analogue) injected i.v. is an alternative.
- However, definitive therapy of varices remains endoscopic obliteration by sclerotherapy.
2. Before abdominal radiography
- AVP/lypressin has been occasionally used to drive out gases from bowel.
Adverse effects
- Because of V2 selectivity, desmopressin produces fewer adverse effects than vasopressin, lypressin or terlipressin.
- However, transient headache and flushing are frequent.
- Nasal irritation, congestion, rhinitis, ulceration and epistaxis can occur on local application.
Systemic side effects are:
- belching, nausea, abdominal cramps, pallor, urge to defecate, backache in females (due to uterine contraction).
- Fluid retention and hyponatraemia may develop.
- Symptoms of hyponatremia are due to shift of water intracellularly resulting in cerebral edema producing headache, mental confusion, lassitude, nausea, vomiting and even seizures.
- Children are more susceptible.
Other Antidiuretics
Thiazides
These drugs are used as diuretics but, exert paradoxical effect (decrease urine formation) in DI.
This paradoxical effect is believed to be due to increased formation of cAMP in the distal tubules. Another proposed mechanism is that thiazides cause dehydration that result in compensatory increase in reabsoprption of Na+ and water from the proximal portions of nephron.
These are low efficacy antidiuretics but are beneficial in both central as well as nephrogenic DI.
Chlorpropamide, Clofibrate and Carbamazepine
These drugs increase the action of ADH on the kidney and are useful only in the central DI.
Amiloride – It is the agent of choice for the treatment of Lithium induced DI.
VASOPRESSIN RECEPTOR ANTAGONISTS
- V1 receptor antagonists may be useful when total peripheral resistance is increased (e.g. CHF and hypertension) whereas
- V2 antagonists may be useful for the treatment of SIADH.
Relcovaptan à selective V1 antagonist
lixivaptan, mozavaptan and tolvaptan à V2 selective antagonists.
Conivaptan is V1a/V2 receptor antagonist à used as an aquaretic (increase water excretion without affecting electrolytes like sodium) in CHF.
Conivaptan is administered by i.v. injection whereas lixivaptan and tolvaptan can be given orally.
SYNDROME OF INAPPROPRIATE ADH SECRETION (SIADH)
- ADH is secreted in response to hypovolemia, in which case its secretion is appropriate.
- However, if ADH is secreted in high quantities in the presence of euvolemia or hypervolemia, it is called inappropriate secretion (SIADH).
- The resultant water retention can result in hyponatremia.
- Thus, SIADH is characterized by normovolemic or hypervolemic hyponatremia.
• Fluid restriction is treatment of choice for SIADH.
• Hypertonic saline (3% NaCl) + loop diuretics (depending upon volume status) is treatment of choice for severe symptomatic hyponatremia.
• Among drugs, tolvaptan (oral), conivaptan (i.v.) are preferred for long-term use.
• Alternatives are demeclocycline and lithium (not preferred now).
