Drugs for Psychiatric Illness
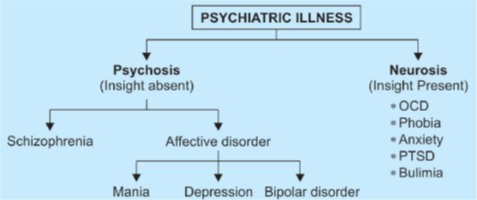
Two major types of psychiatric disorders are psychosis and neurosis.
Psychosis: The patient is not aware of his illness (insight is absent) and refuses to take treatment. It includes major psychosis like schizophrenia as well as mood disorders (like mania, depression and bipolar disorder).
Neurosis: It is less serious and insight is present. It includes anxiety, obsessive-compulsive disorder (OCD), phobias, eating disorders and post-traumatic stress disorder (PTSD).
Antipsychotic Drugs
Schizophrenia is a severe psychiatric illness and is thought to be due to dopaminergic overactivity in the limbic system of the brain.
Other neurotransmitters like 5-HT and NA also probably play a role in this disorder.
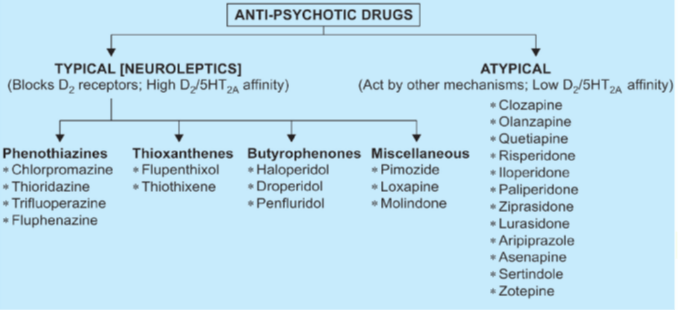
All drugs for schizophrenia have equal efficacy, these mainly differ in potency and can be classified as typical (D2 blockers) and atypical (acting via other mechanisms) antipsychotics.
Actions of Typical Antipsychotics
• These drugs act by blocking D2 receptors and differ significantly in potency. Low potency drugs (like chlorpromazine) are highly sedative whereas high potency drugs cause less sedation.
• High potency drugs are more likely to cause extrapyramidal symptoms (maximum with haloperidol) whereas it is least common with thioridazine.
• High potency drugs have low anticholinergic and autonomic side effects as compared to low potency drugs.
• These drugs lower the seizure threshold and can precipitate convulsions in an epileptic patient.
• All of these agents are potent antiemetic drugs except thioridazine.
• Low potency drugs possess significant α blocking (maximum with chlorpromazine) and anticholinergic (maximum with thioridazine) properties.
High potency compounds have less activity on these receptors.
• Due to the blockade of D2 receptors in the hypothalamus and pituitary, these drugs can increase prolactin release resulting in galactorrhoea and amenorrhea.
Actions of Atypical Antipsychotics
These drugs act by antagonistic actions at 5-HT2 and α receptors and may or may not possess D2 blocking activity.
These drugs are less likely to cause extrapyramidal symptoms.
However, most of these agents (except ziprasidone and aripiprazole) can result in weight gain, hyperlipidemia and new-onset diabetes mellitus.
Tolerance and dependence
Tolerance to the sedative and hypotensive actions develops within days or weeks, but maintenance doses for therapeutic effect in most psychotics remain fairly unchanged over the years, despite increased DA turnover in the brain.
The antipsychotic, extrapyramidal and other actions based on DA antagonism do not display tolerance.
Neuroleptics are hedonically (pertaining to pleasure) bland drugs, lack reinforcing effect so that chronic recipients do not exhibit drug-seeking behavior. Physical dependence is probably absent.
Individual Drugs
• Thioridazine:
- It has the least incidence of extrapyramidal symptoms among typical antipsychotic drugs due to low potency D2 blocking action and the presence of central anticholinergic activity.
- It interferes with male sexual function by inhibiting ejaculation (due to α blocking action)
- It can cause cardiac arrhythmia (Prolongation of QT interval).
- Retinal damage limits long term administration.
Trifluoperazine, fluphenazine, and haloperidol
- These are high potency drugs and have the least α blocking, anticholinergic, sedative and proconvulsant actions. However, extrapyramidal symptoms are marked.
• Penfluridol is the longest acting antipsychotic drug.
• Pimozide selectively blocks D2 receptors without affecting α and muscarinic receptors. It also possesses a long duration of action. It carries the risk of arrhythmias due to QT prolongation.
• Clozapine
- an atypical antipsychotic drug having weak D2 blocking action.
- mainly acts by blocking 5-HT2, alpha-adrenergic and D4 receptors.
- suppresses both positive as well as negative symptoms (First FDA approved drug for antisuicide indication) of schizophrenia.
- It is used only as a reserve drug due to the risk of precipitation of seizures (even in non-epileptics) and agranulocytosis à weekly monitoring of leucocyte count required.
- Convulsions are dose-dependent adverse effect seen only in high doses whereas agranulocytosis is independent of dose.
- Because of association with myocarditis, clozapine is contraindicated in patients with severe heart disease.
- It has powerful anticholinergic effects (equivalent to chlorpromazine and thioridazine).
- Metabolic complication like weight gain, hyperlipidemia, and precipitation of diabetes is another major limitation.
- The risk of extrapyramidal symptoms is least with the use of this drug.
- It specifically has two risks of intestinal dysfunction; potentially severe ileus and sialorrhea.
• Risperidone:
- It acts by blocking 5-HT2, α adrenergic and D2 receptors.
- A more potent D2 blocker than clozapine and can cause extrapyramidal symptoms at a high dose.
- The risk of precipitation of seizures is less than clozapine.
- Hyperprolactinemia has been reported more commonly with risperidone than other atypical antipsychotics.
- Its active metabolite (paliperidone) has a lesser risk of causing metabolic adverse effects.
• Olanzapine:
- It has a similar mode of action as risperidone.
- It is also a potent anticholinergic drug and can cause dry mouth and constipation.
- can cause seizures and weight gain.
- Apart from its use in schizophrenia, it is also used in acute mania and bipolar disorder.
- It has been associated with a significantly higher risk of stroke and death in elderly patients.
• Ziprasidone:
- It causes QT prolongation and carries the risk of arrhythmias.
- Unlike other atypical antipsychotics, it is not associated with weight gain, hyperlipidemia or diabetes.
• Quetiapine: Can cause cataract formation. It has the shortest half-life.
• Aripiprazole:
- Acts as a partial agonist at 5-HT1A and D2 receptors, and antagonist at 5-HT2A receptors.
- It is also known as dopamine- serotonin stabilizer.
- It has quite a long half-life.
- It has also been approved for the treatment of irritability associated with autistic disorders in children.
• Asenapine is used sublingually for schizophrenia and acute mania.
• Iloperidone has less risk of extrapyramidal adverse effects but causes orthostatic hypotension and can prolong QT interval.
Adverse Effects
- CNS
- Drowsiness, lethargy, mental confusion; more with low potency typical antipsychotics Sedation (maximum with chlorpromazine) and some atypical ones like quetiapine and clozapine.
- Tolerance to sedative effects may develop.
- Other side effects are increased appetite and weight gain (not with haloperidol); aggravation of seizures in epileptics; even nonepileptics may develop seizures with high doses of some antipsychotics like clozapine and occasionally olanzapine.
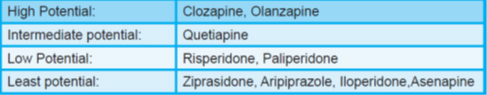
- All atypical antipsychotics may result in weight gain, hyperlipidemia and new-onset diabetes except ziprasidone.
- However high potency, phenothiazines, risperidone, quetiapine aripiprazole, and ziprasidone have little effect on seizure threshold.
According to their potential to cause adverse metabolic side effects, anti-psychotics can be classified as:
- CVS
- Postural hypotension, palpitation, inhibition of ejaculation (especially with thioridazine) are due to α adrenergic blockade; more common with low potency phenothiazines.
- Q-T prolongation and cardiac arrhythmias à risk of overdose with thioridazine, pimozide, and ziprasidone.
- Anticholinergic
- Dry mouth, blurring of vision, constipation, urinary hesitancy in elderly males (thioridazine has the highest propensity); absent in high potency agents.
- Some like clozapine induces hypersalivation despite anticholinergic property, probably due to central action.
- Endocrine
- Hyperprolactinemia (due to D2 blockade) is common with typical neuroleptics and risperidone.
- amenorrhoea, infertility, galactorrhoea, and gynecomastia occur infrequently after prolonged treatment.
- The atypical antipsychotics, except risperidone, do not appreciably raise prolactin levels.
- Metabolic effects
- Elevation of blood sugar and triglyceride levels as a consequence of chronic therapy with certain antipsychotics is a major concern now.
- Low potency phenothiazines (CPZ, thioridazine) and some atypical antipsychotics, particularly olanzapine and clozapine have a high risk of precipitating diabetes or worsening it.
- High potency drugs like trifluoperazine, fluphenazine, haloperidol and atypical antipsychotics like risperidone, aripiprazole and ziprasidone have low/no risk.
- The mechanism of this effect is not clear; maybe due to weight gain and/or accentuation of insulin resistance.
- Extrapyramidal disturbances
- major dose-limiting side effects; more prominent with high potency drugs like fluphenazine, haloperidol, pimozide, etc.,
- least with thioridazine, clozapine, and all other atypical antipsychotics, except a higher dose of risperidone. The extrapyramidal effects may be categorized into:
(a) Parkinsonism with typical manifestations—
- rigidity, tremor, hypokinesia, mask-like facies, shuffling gait
- appears between 1–4 weeks of therapy and persists unless the dose is reduced.
- If that is not possible, one of the anticholinergic antiparkinsonian drugs may be given concurrently.
- Changing the antipsychotic, especially to an atypical agent, may help.
- Though quite effective, a routine combination of the anticholinergic from the start of therapy in all cases is not justified, because they tend to worsen memory and impair intellect, in addition to dry mouth and urinary retention.
- Amantadine is an alternative.
- A rare form of extrapyramidal side effect is perioral tremors ‘rabbit syndrome’ that generally occurs after a few years of therapy à often responds to central anticholinergic drugs.
(b) Acute muscular dystonias
- Bizarre muscle spasms, mostly involving linguo-facial muscles —grimacing, tongue thrusting, torticollis, locked jaw; occurs within a few hours of a single dose or at the most in the first week of therapy.
- It is more common in children below 10 years and in girls, particularly after parenteral administration; overall incidence is 2%.
- It lasts for one to a few hours and then resolves spontaneously.
(c) Akathisia
- Restlessness, feeling of discomfort, apparent agitation manifested as a compelling desire to move about, but without anxiety
- seen in some patients between 1–8 weeks of therapy: up to 20% incidence.
- maybe mistaken for exacerbation of psychosis.
- A central anticholinergic may reduce the intensity in some cases, but a benzodiazepine like clonazepam or diazepam is the first choice treatment of motor restlessness.
- Propranolol is more effective; may be given to non-responsive cases.
- Most patients respond to a reduction in dose of the neuroleptic or changeover to an atypical antipsychotic like quetiapine.
(d) Malignant neuroleptic syndrome
- It occurs rarely with high doses of potent agents.
- the patient develops marked rigidity, immobility, tremor, hyperthermia, semiconsciousness, fluctuating BP and heart rate; myoglobin may be present in the blood.
- The syndrome lasts 5–10 days after drug withdrawal and may be fatal.
- The neuroleptic must be stopped promptly and symptomatic treatment instituted.
- Intravenous dantrolene may benefit.
(e) Tardive dyskinesia
- occurs late in therapy, sometimes even after withdrawal of the neuroleptic: manifests as purposeless involuntary facial and limb movements like constant chewing, pouting, puffing of cheeks, lip licking, choreoathetoid movements.
- more common in elderly women, and is a manifestation of progressive neuronal degeneration along with supersensitivity to DA.
- An incidence of 10–20% has been reported after long term treatment.
- Miscellaneous
- Weight gain often occurs due to long-term antipsychotic therapy,
- sugar and lipids may tend to rise.
- Blue pigmentation of exposed skin, corneal and lenticular opacities, retinal degeneration (more with thioridazine)
- Hypersensitivity reactions
- Cholestatic jaundice with portal infiltration; 2–4% incidence; occurs between 2–4 weeks of starting therapy à More common with low potency phenothiazines; rare with haloperidol.
- Skin rashes, urticaria, contact dermatitis, photosensitivity (more with CPZ).
- Agranulocytosis is rare; more common with clozapine.
- Myocarditis Few cases have occurred with clozapine.
- Cataract formation with quetiapine.
Other Uses
• These agents can be used as an alternative to ECT in severe depression with psychotic features.
• Alcoholic hallucinosis.
• Gilles de la Tourette’s syndrome and Huntington’s disease (Haloperidol is the drug of choice).
Note:
1. Haloperidol and fluphenazine are the most potent typical antipsychotic drugs whereas risperidone is the most potent atypical antipsychotic agent.
2. The risk of extrapyramidal adverse effects is negligible with clozapine, quetiapine, and aripiprazole.
3. Chlorpromazine, thioridazine, and clozapine possess the strongest anticholinergic activity.
4. Fluphenazine (enanthate and decanoate) and haloperidol (decanoate) are long-acting injectable (s.c. or i.m) forms of typical antipsychotics.
Risperidone is the first atypical antipsychotic available in long-acting injectable form.
5. The most commonly used antipsychotic by the intravenous route is haloperidol. l Nervous System
6. Ziprasidone, aripiprazole, asenapine, and iloperidone has negligible risk to cause metabolic adverse effects (weight gain, hyperlipidemia, and new-onset diabetes mellitus)
7. Asenapine, paliperidone, and ziprasidone have the greatest potential to prolong the QT interval.
