Drug dependence
Repeated administration of certain drugs may induce a habit and dependence.
If the habit-forming agent is not made available to the habitué, he develops withdrawal symptoms characterized by psychic/physical disturbances like headache, restlessness & emotional upset and/or convulsions & vasomotor collapse.
WHO definition à, ‘A state, psychic & sometimes also physical, resulting from the interaction between a living organism & a drug, characterized by behavioral & other responses that always include a compulsion to take the drug on a continuous or periodic basis in order to experience its psychic effects & sometimes to avoid the discomfort of its absence.
Tolerance may or may not be present. A person may be dependent on more than one drug’. Withdrawal of a drug can precipitate a drug withdrawal syndrome.
Drug dependence is of 3 type:
- Psychic: A condition in which a drug produces ‘a feeling of satisfaction & a psychic drive that require periodic or continuous administration of the drug to produce pleasure or to avoid discomfort’, is called psychic dependence.
- Physical: In the case of physical dependence, the body achieves an adaptive state that manifests itself by intense physical disturbances when the drug is withdrawn (withdrawal syndrome).
- Combined.
Drugs causing dependence include
- Opioids: Morphine, Heroin, Pethidine (Psychological + Physical)
- CNS Stimulants: Amphetamjines, Methylphenidate, Caffeine, Nicotine, Cocaine
- CNS Depressants: Ethyl alcohol, Barbiturates, Benzodiazepines, Methaqualone
- Hallucinogens: Lysergic acid diethylamide (Only Psychological), Phencyclidine, Cannabinoids,
Psilocybine, Psilocin, Dimethyl tryptamine,
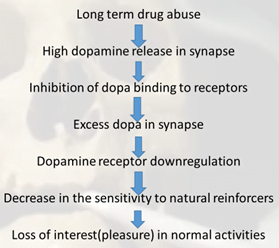
Role of Dopamine
- Primary neurotransmitter of the reward circuit in the brain.
- It regulates movement, emotion, cognition, motivation, and feelings of pleasure.
- Natural Rewards like food, water, coitus, nurturing etc. cause a release of dopamine, and are associated with the reinforcing nature of these stimuli.
- Nearly all addictive drugs, directly or indirectly, act upon the brain’s reward system by flooding the circuit with dopamine.
- On drug abuse, dopamine secretion can increase from 2 to 10 folds. Thus, addictive drugs are perceived by the brain as being very rewarding, this can lead to repetitive behavior (reinforcement).
- Opioids
Overdose à Accidental, suicidal or seen in drug abusers
S/S: respiratory depression, cyanosis, fall in BP and shock, miosis, flaccidity, stupor, coma, death due to respiratory failure
Treatment:
Respiratory support, maintenance of BP, gastric lavage
Specific antidote: Naloxone 0.4-0.8 mg i.v.
Opioid Dependence
Most individuals with Opioid Dependence have significant levels of tolerance.
Withdrawal is associated with marked drug seeking behaviour
Physical manifestations à lacrimation, sweating, yawning, anxiety, fear, restlessness, mydriasis, tremor, insomnia, abdominal colic, diarrhoea, rise in BP, palpitation, rapid weight loss
Treatment:
- Substitution therapy with methadone
- Clonidine: α2 agonist acts on presynaptic receptors & inhibit release of NE
- Naltrexone + Clonidine: naltrexone induces withdrawal which is overcome by clonidine, then naltrexone is used for maintenance
- Cannabinoids
Obtained from Cannabis indica (marijuana)
Various forms in which it is used:
- Bhang derived from dried leaves, taken orally
- Ganja derived from dried female inflorescence, smoked
- Charas resinous extract from flowering tops and leaves, smoked with tobacco (hashish)
- Most important active principle isΔ9 tetrahydrocannabinol (Δ9 THC)
Cannabis Dependence
- Individuals with dependence have compulsive use & generally do not develop physiological dependence.
- Chronic use leads to tolerance
- Withdrawl symptoms – mild
- Interferes with family, school, work or recreational activities. (amotivational syndrome)
- Persistent use despite physical (e.g chronic cough d/t smoking) or psychological (e.g excess sedation d/t repeated use of high doses)
- Supportive treatment suffice in withdrawal state.
- Hallucinogens
Affect thought, perception and mood at low doses with minimal effects on memory & orientation
Produce shape and color distortion, depersonalization, hallucination, slowing of time perception, sense that colors are heard & sounds are seen
- Hallucinogens may continue to be used despite the knowledge of adverse effects (e.g., memory impairment while intoxicated; “bad trips,“ which are usually panic reactions; or flashbacks)
- Bad trips require medical attention in form of talking down/reassurance.
- Severe agitation may respond to diazepam (20 mg orally)
- Nicotine and tobacco
Spending a great deal of time in using the substance is best exemplified by chain-smoking. (time to procure is minimal)
Giving up important social, occupational, or recreational activities (in searching smoking-restricted areas)
Continued usage despite medical problems like bronchitis, COPD d/t smoking.
- Combination of psychological and pharmacological treatment
- Nicotine replacement therapy: transdermal patch, chewing gum, inhalers, nasal spray, lozenges
- Bupropion, Clonidine
- Rimonabant : CB1receptor inverse agonist improves abstinence rates and reduces the weight gain but high frequency of depressive and neurologic symptoms
- Varenicline : partially stimulates nicotinic receptors – reducing craving and preventing most withdrawal symptoms.
- Alcohol (ethanol)
- Acts through several cellular mechanisms
- Ionotropic receptors:
GABAA – enhances GABA mediated inhibition,
NMDA (glutaminergic) – inhibition
5-HT3 – activation
- Ion channel: Kir3/GIRK
- Transporter: (equilibrative nucleoside transporter, ENT1, related to adenosine uptake)
- Not known which target is responsible for DA release
- Anti-craving agents
- Naltrexone: interferes with alcohol induced reinforcement by blocking opioid receptors
- Acamprosate : NMDA receptor antagonist – normalize the dysregulated neurotransmission associated with chronic ethanol intake
- Fluoxetine: used occasionally
- Amphetamines dependence treatment
- Behaviour therapy: aversion therapies like sub threshold electric shock or emetic like apomorphine
- Psychotherapy
- Group therapy e.g. alcoholics anonymous, narcotic anonymous
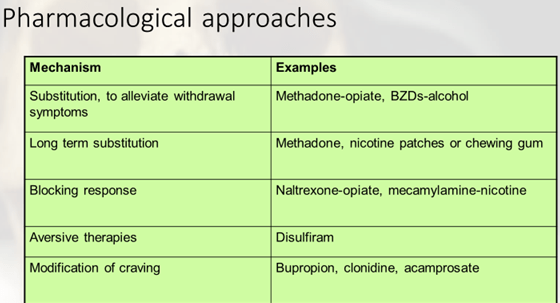
- Detoxification: Gradual tapering of drug that has caused dependence or sudden withdrawal of drug followed by substitution therapy
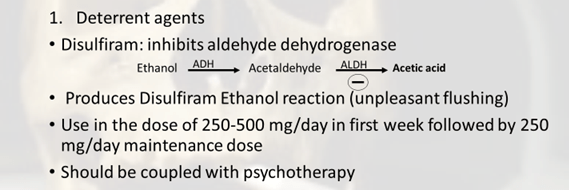
- Specific drug therapy e.g. Disulfiram
- Correction of nutritional deficiencies
- Community treatment and rehabilitation