Drug Therapy Of Migraine
- characterized by pulsating headache, usually restricted to one side, which comes in attacks lasting 4-48 hours and is often associated with nausea, vomiting, sensitivity to light and sound. flashes of light, vertigo, loose motions and other symptoms.
- Two major types are-
- migraine with aura (classical migraine) à headache is preceded by visual or other neurological symptoms, and
- migraine without aura (common migraine).
Pulsatile dilatation of certain large cranial vessels is the immediate cause of pain.
Pathogenic mechanisms
Vascular theory
initial vasoconstriction or shunting of blood through carotid arterio-venous anastomoses produces cerebral ischemia and starts the attack.
Neurogenic theory
spreading depression of cortical electrical activity followed by vascular phenomena.
Some triggering event à produce neurogenic inflammation of the affected blood vessel wall à and release of mediators like 5-HT, neurokinin, substance P, calcitonin gene related peptide (CGRP), nitric oxide, etc.
- Migraine involves the trigeminal nerve distribution to intracranial arteries
- These nerves release peptide neurotransmitters à especially calcitonin gene related peptideà extremely powerful vasodilator à also, increases glutamate activation of AMPA receptors
- TRPV1 receptors play an important role in à modulating trigeminal sensory processing and this have been proposed as potential targets for migraine treatment.
- Substance P and Neurokinnin A may also be involved.
- Vasodilatation results in extravasation of plasma and plasma proteins into the perivascular space leading to edema
- The mechanical stretch then caused by the perivascular edema is the cause of activation of pain nerve endings in the duramater.
The International Classification of Headache Disorders, 3rd edition (ICHD-3) specifies diagnostic criteria for migraine
| Migraine without aura |
| A. At least five attacks fulfilling criteria B through D |
| B. Headache attacks lasting 4 to 72 hours (untreated or unsuccessfully treated) |
| C. Headache has at least two of the following characteristics: |
| Unilateral location |
| Pulsating quality |
| Moderate or severe pain intensity |
| Aggravation by or causing avoidance of routine physical activity (eg, walking or climbing stairs) |
| D. During headache at least one of the following: |
| Nausea, vomiting, or both |
| Photophobia and phonophobia |
| E. Not better accounted for by another ICHD-3 diagnosis |
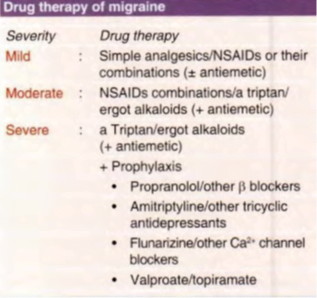
Mild migraine
fewer than one attack per month of throbbing but tolerable headache lasting upto 8 hours which does not incapacitate the individual
- Simple analgesics
- paracetamol (0.5-1 g) or
- aspirin (300-600 mg) and repeated 4-6 hourly abort and suppress most mild attacks
(ii) Nonsteroidal anti-inflammatory drugs (NSAIDs) and their combinations
- ibuprofen (400- 800 mg 8 hourly),
- naproxen (500 mg followed by 250 mg 8 hourly),
- diclofenac (50 mg 8 hourly),
- mephenamic acid (500 mg 8 hourly),
- indomethacin (50 mg 6- 8 hourly) either alone or combined with paracetamol/codeine/ diazepam or another sedative/diphenhydramine or another antihistaminic/caffeine
- Dispersible or effervescent formulations à should be preferred , because gastric stasis attending migraine attack may hamper absorption from the regular tablet.
- Analgesics are more effective in migraine without aura,
- taken only till the attack passes off. Excessive use of analgesic may itself cause headache.
- Long term treatment on a regular schedule to ward off migraine attacks is not advised.
- Antiemetics
- Gastric stasis occurs during migraine which delays absorption of oral drugs.
- Metoclopramide (10 mg oral/ i.m.) is frequently used.
- relieves nausea, vomiting and gastric stasis
- Domperidone ( I 0- 20 mg oral) and prochlorperazine ( I 0-25 mg oral/ i.m.) are also effective.
- Diphenhydramine or promethazine exert sedative as well as antiemetic action.
Moderate migraine
throbbing headache is more intense, lasts for 6-24 hours, nausea/ vomiting and other features are more prominent and the patient is functionally impaired. One or more attacks occur per month.
Simple analgesics are usually not effective,
stronger NSAlDs or their combinations mentioned above are beneficial in many cases.
The remaining are treated with a specific antimigraine drug, i.e. a triptan or an ergot preparation.
Antiemetics are almost regularly needed.
Prophylactic therapy is advised only when attacks are more frequent than 2- 3 per month.
Severe migraine
patients suffer 2- 3 or more attacks per month of severe throbbing headache lasting 12-48 hours, often accompanied by vertigo, vomiting and other symptoms; the subject is grossly incapacitated during the attack.
Analgesics/NSAIDs and their combinations à usually do not afford adequate relief-
Specific antimigraine drugs have to be prescribed along with antiemetics.
Combination of a longer acting analgesic like naproxen with a triptan may be more suitable for patients who have prolonged migraine attacks and suffer recurrences when treated with a triptan alone.
Prophylactic regimens lasting 6 months or more are recommended.
SPECIFIC ANTIMIGRAINE DRUGS
Ergotamine
- most effective ergot alkaloid for migraine.
- Given early in attack, lower doses generally suffice, and relief is often dramatic.
- Oral/ sublingual route is preferred, 1 mg is given at half hour intervals till relief is obtained or a total of 6 mg is given.
- Parenteral administration, though rapid in action is more hazardous.
- acts by constricting the dilated cranial vessels and/or by specific constriction of carotid A-V shunt channels
- reduce neurogenic inflammation and leakage of plasma in duramater that occurs due to retrograde stimulation of perivascular afferent nerves à mediated via à partial agonism at 5-HT 1B/1D receptors in and around cranial vessels.
Dihydroergotamine (DHE)
- nearly as effective as ergotamine and
- preferred for parenteral administration because injected DHE is less hazardous.
Current status
- rarely used now, except for considerations of cost or when triptans fail
- Because of erratic oral absorption, frequent side effects, especially nausea, vomiting, muscle cramps and availability of triptans
- no prophylactic value à regular use is not justified
Caffeine 100 mg taken with ergotamine enhances its absorption from oral and rectal routes and adds to the cranial vasoconstricting action.
Selective 5-HT 1B/1D agonists (Triptans)
- selectively activate 5-HT 1B/1D receptors, and are called ‘triptans’
- Currently à first line drugs for patients who fail to respond to analgesics.
- Ergot alkaloids are now required only in few cases.
Because these drugs have been designed to act on the same subtype of5-HT receptor, pharmacodynamic differences among them are minor, but there are significant pharmacokinetic differences.
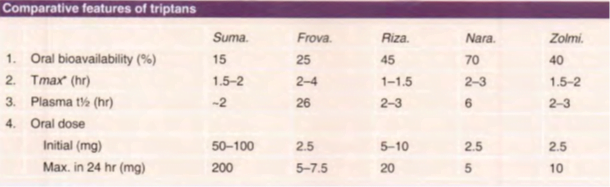
- All others triptans have higher oral bioavailability than the prototype drug sumatriptan.
- Fewer headache recurrences in an attack are reported with naratriptan and frovatriptan due to their longer t½, but they may be slower in affording initial pain relief
- The use of sumatriptan (or other triptans) should be restricted to treatment of acute attacks of moderate to severe migraine not responding to analgesics or their combinations.
Sumatriptan
- first selective 5-HT 1B/1D receptor agonist; activates other subtypes of 5-HT1 receptors only at very high concentrations
- only triptan available for nasal and parenteral administration as well
- Administered at the onset of an attack of migraine, sumatriptan is as effective and better tolerated than ergotamine.
- About 3/4 patients obtain complete/significant relief within 2-3 hours.
- However, recurrence of headache within 24 hr has been noted in 20-40% patients, probably due to short t½ of sumatriptan.
- A distinct advantage à tends to suppress nausea and vomiting of migraine, while ergotamine accentuates these symptoms.
MOA à 5-HT 1B/1D receptor mediated constriction of dilated cranial blood vessels, especially the arterio-venous shunts in the carotid artery, which express 5-HT10110 receptors.
Dilatation of these shunt vessels during migraine attack is believed to divert blood flow away from brain parenchyma.
5-HT 1B/1D receptors are presynaptic autoreceptors à sumatriptan can reduce 5-HT release at these
blood vessels.
in addition à may inhibit inflammatory neuropeptide release around the affected vessels as well as extravasation
of plasma proteins across dural vessels.
suppress neurogenic inflammation of cranial vessels.
Pharmacokinetics:
Sumatriptan is absorbed rapidly and completely after s.c. injection.
Oral bioavailability averages only 15%.
Absorption is faster after intranasal spray, but bioavailability remains almost the same.
Side effects of sumatriptan are usually mild.
- Tightness in head and chest, feeling of heat and other paresthesias in limbs, dizziness, weakness are short lasting, but dose related side effects.
- These are more common after s.c. injection, which is painful.
- Slight rise in BP occurs, but has little clinical relevance, because sumatriptan is not a drug for regular use.
- Bradycardia, coronary vasospasm and risk of myocardial infarct ion are the serious, but infrequent adverse effects.
- Seizures and hypersensitivity reactions are rare.
Contraindications:
- lschaemic heart disease, hypertension, epilepsy, hepatic or renal impairment and pregnancy are the contraindications.
- Patients should be cautioned not to drive.
- Sumatriptan and ergotamine should not be administered within 24 hours of each other.
Dose: 50- 100 mg oral al the onset or migraine attack, may be repeated once within 24 hours if required.
6 mg s.c. may be given to patients who cannot take the drug orally or in whom the pain develops very rapidly.
25 mg nasal spray can be used
combination of sumatriptan (a migraine-specific triptan) and naproxen (an anti-inflammatory pain reliever) in a single tablet for the acute treatment of migraine.
FDA Approved: Yes (First approved April 15, 2008)May 15, 2015 FDA Approves Treximet (sumatriptan and naproxen sodium) for Migraine in Pediatric
Rizatriptan:
more potent, has higher oral bioavailability with slightly faster onset of action.
Dose: 5-1 0 mg
Naratriptan. Zolmitriptan, Almotriptan, Frovatriptan and Eletriptan are other triptans used in some countries.
PROPHYLAXIS OF MIGRAINE
- moderate-to-severe migraine when 2- 3 or more attacks occur per month, or
- when attacks are disabling despite treatment, or
- in patients with contraindications for triptans/ergotamine.
Diverse classes of drugs are used, but none is effective in all cases, and none abolishes the attacks totally.
Discontinue prophylaxis every 6 months to check whether its continuation is needed or not. It is important
to avoid the precipitating factor(s).
- beta-Adrenergic blockers à Propranolol
- most commonly used drug.
- reduces frequency as welI as severity of attacks in upto 70% patients.
- Effect is generally seen in 4 weeks and is sustained during prolonged therapy.
- starting dose à 40 mg BD, which may be increased upto 160 mg BD if required.
MOAà is not clear
- Other nonselective (timolol} and beta1 selective (metoprolol, atenolol) agents are also effective, but pindolol and others having intrinsic sympathomimetic action are not useful.
- Tricyclic antidepressantsà amitriptyline (25-50 mg at bed time)
- has been most extensively tried, reduce migraine attacks.
- effective in many patients but produces more side effects than propranolol.
- Whether its 5-HT (and other monoamine) uptake blocking property is causally related to the prophylactic effect is not known.
- The antimigraine effect is independent of antidepressant property
- This class of drugs are better suited for patients who concurrently suffer from depression.
(iii) Calcium channel blockersà Verapamil
- reduce migraine attacks à inferior to propranolol.
Flunarizine à relatively weak Ca2+ channel blocker that inhibits Na+ channels as well.
- Claimed as effective as propranolol, but convincing proof is lacking.
- cerebro-selective Ca2+ channel blocker, which may benefit migraine by reducing intracellular Ca2+ overload due to brain hypoxia and other causes.
- Side effects à sedation, constipation, dry mouth, hypotension, flushing. weight gain.
(iv) Anticonvulsantsà Valproic acid ( 400-1200 mg/day) and gabapentin (300- 1200 mg/day)
- have some prophylactic effect in migraine.
- newer drug topiramatehas recently been approved for migraine prophylaxis.
- 50% reduction in the number of attacks in half of the patients was noted in 2 randomized trials.
- topiramate 25 mg OD and gradually increase to 50 mg OD or BD.
- Efficacy of anticonvulsants in migraine is lower than that of beta blockers.
- indicated in patients refractory to other drugs or when propranolol is contraindicated.
(v) CGRP antagonist – Erenumab
- fully human monoclonal antibody – blocks calcitonin gene-related peptide (CGRP) receptor
- recently found to reduce number of migraine attacks when injected s.c. once a month in patients with severe migraine
- approved by US-FDA.
(vi) 5-HT antagonists à methysergide and cyproheptadine
less impressive than beta blockersà not used now for migraine.
Selection of drug for prophylaxis:
- For patients with hypertension who are nonsmokers and ≤60 years of age, reasonable options àmetoprolol, propranolol, or timolol in the absence of contraindications to beta blockers.
- For patients with hypertension who are smokers or are >60 years of age, options include verapamil or flunarizine.
using beta blockers as initial therapy for migraine prevention in these patients à may be associated with a higher rate of stroke and other cardiovascular events
●For patients with depression or mood disorderà include amitriptyline or venlafaxine.
●For patients with epilepsy, à valproate or topiramate.
●For patients with insomnia àamitriptyline is a reasonable option.
●For patients with obesity à topiramate is a reasonable option.
●For patients with Raynaud phenomenonà verapamil or flunarizine.
Recent advances in migraine
- CGRP antagonists (Telcagepant and olcagepant)
- The calcitonin gene-related peptide (CGRP) is a therapeutic target in migraine because of its hypothesized role in mediating trigeminovascular pain transmission and the vasodilatory component of neurogenic inflammation.
- development of telcagepant was stopped à hepatotoxicity, and
- development of olcegepant was halted à poor oral bioavailability
Erenumab (2018)
human monoclonal antibody that binds to and inhibits the CGRP receptor – for prophylaxis
Fremanezumab — (September 2018)
human monoclonal antibody that binds to both isoforms of the CGRP ligand, appears to be modestly effective for prevention of episodic migraine.
Galcanezumab à a human monoclonal antibody that binds to the CGRP ligand
- May 15, 2015 àFDA Approves Treximet (sumatriptan and naproxen sodium) for Migraine in Pediatric Patients
- 5HT1F agonist: Lasmiditan (completed two Phase III randomized)
- MOA: inhibits trigeminal nucleus Fos activation and decreases neuronal activation and neuronal firing.
- No direct vasoconstrictor activity of self.
- lasmiditan had a relatively high rate of serious adverse events, particularly at higher doses; the most common were dizziness, fatigue, vertigo, paresthesia, and somnolence
- Gap junction inhibitor – Tonabersat (not approved)
selectively binding and blocking glial cell gap junction activity and thus interfering with excitation of nearby trigeminal neurons and propagation of cortical depolarization
There was a lack of evidence to support use of tonabersat for migraine prophylaxis
- Vanilloid TRPV1 receptor antagonists – SB-705498
TRPV1 receptors play an important role in à modulating trigeminal sensory processing and this have been proposed as potential targets for migraine treatment.
prevent and reverse central sensitization
- Glutamate receptor antagonists: Tezampanel
- Glutamate is excitatory NT. There are 3 types of ionotropic glutamate receptors. Glutamate plays a role in migraine pathophysiology. (decreases central sensitization and CSD)
- nNOS inhibitors and 5HT1B/1D agonist: triptans increase expression of nNOS, hence this combination is being tested
- PG EP4 receptor antagonist: might not be more effective than NSAIDS
- Transcranial magnetic stimulation and transcranial direct stimulation
- New delivery systems
- Sumatriptan rectal route: bypass nausea
- Sumatriptan intranasal route: but absorbed by gut: Bypass nausea
Tosymra (sumatriptan nasal spray) àApproved January 2019
Specific Treatments: acute migraine in adults
The efficacy of Tosymra was based on the relative bioavailability of Tosymra nasal spray compared to sumatriptan subcutaneous injection (4 mg) in healthy adults
- Ultrafine sumatriptan for pulmonary delivery
- Transdermal sumatriptan: bypass nausea
- January 2013, FDA approved: acute medication sumatriptan delivery by new mechanism (transdermal patch)
- ADR: Painful sensation at the patch application site
- Intranasal DHE
- FDC
- 85 mg of sumatriptan with 500 mg of naproxen approved by FDA
- Triptan with caffeine and triptan with PCM are being tested
- Recent advances for migraine prophylaxis
- Onabotulinum toxin A (2010)
- MOA: synaptobrevin, syntaxin, SNAP-25. The light chain of toxin inhibits SNAP-25
- Drugs in development: Ethosuximide, Lacosamide, iNOS inhibitor, Ramelteon.
Cerena
- 13 December 2013: FDA allowed marketing of first device to relieve migraine headache pain (Cerena)
- Device delivers Pulse transcranial magnetic stimulation at the onset of headache or aura
Disrupts cortical spreading depression
Cefaly
- 11 March 2014: USFDA approved device for preventing migraine.
- Transcutaneous Electrical Nerve Stimulator to Treat Headache
- Warnings: Indicated for use by adults and should only be used for 20 minutes/day
- ADR: Tingling or massaging sensation where electrode applied.

