RENIN-ANGIOTENSIN SYSTEM
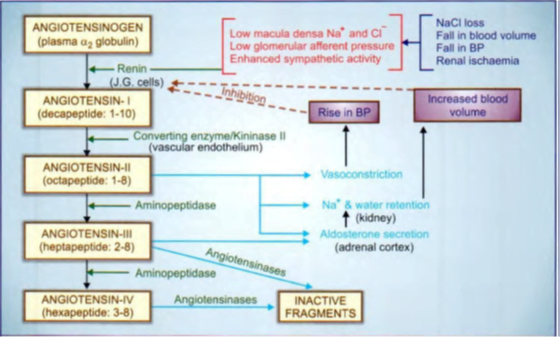
Precursor plasma α2 globulin à angiotensinogen à inactive decapeptide angiotensin-1 (Ang I)
The plasma t½ of renin is 15 min, Circulating Ang II also has a very short t½ (1 min).
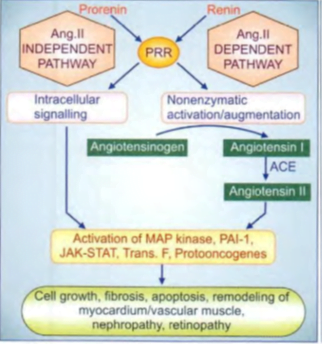
Prorenin and (Pro) renin receptor (PRR)
- Renin is synthesized in the juxtaglomerular (JG) cells of the kidney and in tissues expressing local RAS as a larger peptide pre-prorenin.
- appropriate stimuli à both prorenin and renin are secreted; the former inn much larger quantities. The concentration of prorenin in circulation is 5-10 folds higher than that of renin.
- Till recently, prorenin was considered to be only the inactive precursor of renin, but now it is recognized to be active in its own right.
- Nonenzymatic and reversible activation occurs by binding of prorenin to another trans-membrane protein called (Pro) renin receptor (PRR).
- prorenin exerts effects via Ang II-dependent and Ang II independent pathways
- Ang II independent pathway: Binding of prorenin/renin to PRR on cell surface directly triggers intracellular signaling via activation of MAP kinase, plasminogen activator-inhibitor- I JAK-STAT pathway, transcription factors, protooncogenes, etc. to regulate cell growth, collagen deposition, fibrosis, and apoptosis.
Overactivity of RAS
- contributes to pathological changes and end-organ damage in many conditions like hypertensive vascular and ventricular hypertrophy, post-infarction myocardial fibrosis, and remodeling, congestive heart failure, nephropathy, retinopathy, etc.
ACTIONS
- CVS
- The most prominent action of Ang II à vasoconstrictionà produced directly as well as by enhancing Adr/ NA release from adrenal medulla/adrenergic nerve endings and by increasing central sympathetic outflow.
- In addition, Ang II inhibits the reuptake of NA and augments the responsiveness of vascular smooth muscle to it.
- Vasoconstrictionà arterioles, and venules and occurs in all vascular beds.
- Promotes movement of fluid from vascular to extravascular compartment.
- Ang II increases the force of myocardial contraction by promoting Ca2+ influx.
- Increase heart rate by enhancing the sympathetic activity, but this is opposed by the reflex effect of a rise in BP.
- Cardiac output is often reduced and cardiac work is increased (due to the rise in peripheral resistance).
- Ang II acting on a chronic basis à hypertrophy, hyperplasia and increased intercellular matrix production in the myocardium as well as vascular smooth muscle
- Long-standing hypertension increases vessel wall as well as intimal thickness and causes ventricular hypertrophy.
- Fibrosis and dilatation of the infarcted area with hypertrophy of the non-infarcted ventricular wall are seen after myocardial infarction.
- Progressive cardiac myocyte death and fibrotic transformation occur in CHF.
ACE inhibitor therapy retards/reverses many of these changes imparting a pivotal role to Ang II in vascular and ventricular hypertrophy, apoptosis and remodeling.
2. Adrenal cortex: Enhance synthesis and release of aldosterone à promote Na+ reabsorption and K+/H- excretion.
3. Kidney: promotes Na+/H+ exchange in proximal tubule àincreased Na+, Cl- and HC03 reabsorption. Ang II reduces renal blood flow and GFR and produces intrarenal hemodynamic effects which normally result in Na+ and water retention.
Specific Ang II receptors are expressed on the surface of target cells. Two subtypes (AT1 and AT2) have been differentiated pharmacologically: Losartan is a selective AT1 antagonist.
However, all major effects of Ang II are mediated by the AT1 receptor
4. Electrolyte, blood volume, and pressure homeostasis
Changes that lower blood volume or blood pressure, or decrease Na+ content induce renin release by three mechanisms.
• Intrarenal baroreceptor pathway: By decreasing tension in the afferent glomerular arterioles, it operates partly through increased production of prostaglandins (PGE2), nitric oxide, etc, and partly via stretch sensitive ion channels.
• Macula densa pathway: COX-2 and neuronal nitric oxide synthase (nNOS) are induced in macula densa cells by Na+ depletion -> release of PGE2 and PGI2 is enhanced both due to increased amount of COX-2 as well as its activation by NO.
The locally released PGs act on juxtaglomerular cells to promote renin secretion.
• β3 adrenoceptor pathway: Baroreceptor and other reflexes that increase sympathetic impulses to JG cells activate β1 adrenoceptors expressed on their surface à increased intracellular cAMP triggers renin release.
Increased renin is translated into increased plasma Ang II which produces an acute rise in BP
The rise in BP, in turn, inhibits renin release: the long loop negative feedback mechanism.
A short-loop negative feedback mechanism operates within the kidney: activation of AT1 receptors on JG cells inhibits renin release directly.
The mechanisms of regulation of renin release have important pharmacological implications:
• ACE inhibitors and AT1 antagonists enhance renin release by interfering with both the short-loop and long-loop negative feedback mechanisms.
• Vasodilators and diuretics stimulate renin release by lowering BP.
• Loop diuretics increase renin production by reducing the entry of Na+ and Cl into macula densa cells.
Inhibition of the renin-angiotensin system
I. Sympathetic blockers (beta-blockers, adrenergic neuron blockers, central sympatholytics)- decrease renin release.
2. Direct renin inhibitors (DRls, e.g. aliskiren):
3. Angiotensin-converting enzyme (ACE) inhibitors (e.g. captopril)
4. Angiotensin receptor blockers (ARBs, e.g. losartan)- antagonize the action of Ang II on target cells.
5. Aldosterone antagonists (e.g. spironolactone) à block mineralocorticoid receptors.
ACE Inhibitors
- Captopril à first orally active ACE inhibitor
- enalapril, lisinopril, benazepril, ramipril, fosinopril, quinapril, trandolapril, imidapril and perindopril.
Captopril- prototype
- abolishes the pressor action of Ang I but not that of Ang II: It does not block AT1 or AT2 receptors.
- ACE is a relatively nonspecific enzyme; splits off a dipeptidyl segment from several peptides including bradykinin, substance P, a natural stem cell regulating peptide, enkephalins, etc. in addition to Ang I.
- elevated kinins (and PGs whose synthesis is enhanced by kinins) à responsible for cough and angioedema induced by ACE inhibitors in susceptible individuals.
- Fall in BP by ACE Inhibitors is more marked when Na+ has been depleted by dietary restriction or diuretics because the renin level is high.
- Treatment with ACE inhibitors causes feedback increase in renin release resulting in overproduction of Ang I. Since its conversion to Ang II is blocked, Ang I is diverted to produce more Ang ( I-7) which has vasodilator property, and could contribute to the BP-lowering action of ACE inhibitors.
- The arterioles dilate and compliance of larger arteries is increased à decrease in total peripheral resistance -> Both systolic and diastolic BP fall.
- Cardiovascular reflexes are not interfered -> little dilatation of capacitance vessels à postural hypotension is not a problem.
- Reflex sympathetic stimulation does not occur despite vasodilatation à can be safely used in patients with ischaemic heart disease
- Cerebral and coronary blood flow is also not compromised.
- renal blood flow is not compromised à due to greater dilatation of renal vessels
Adverse effects
• Hypotension: An initial sharp fall in BP occurs especially in diuretic treated and CHF patients; persistent hypotension may be troublesome in MI patients.
• Hyperkalaemia: à likely in patients with impaired renal function and in those taking K+ sparing diuretics, NSAIDs or beta-blockers.
• Cough: A persistent brassy cough occurs in 10- 16% patients within 1- 8 weeks, often requires discontinuation of the drug-subsides 4- 6 days thereafterà not dose-related and appears to be caused by inhibition of bradykinin/ substance P breakdown in the lungs of susceptible individuals.
• Rashes, urticaria: Occur in 1-4% recipients; Angioedema is rare.
• Dysgeusia: Reversible loss or alteration of taste sensation due to captopril, rarely with other ACE inhibitors.
• Foetopathic: Foetal growth retardation, hypoplasia of organs and fetal death may occur if ACE inhibitors are given during later half of pregnancy. ACE inhibitors must be stopped when the woman conceives.
• Headache, dizziness, nausea, and bowel upset: in 1-4 % patients.
• Granulocytopenia and proteinuria: Renal disease predisposes to these adverse effects.
However, ACE inhibitors retard diabetic nephropathy, reduce attendant proteinuria, and are reno-protective.
• Acute renal failure: may be precipitated in patients with bilateral renal artery stenosis due to a fall in glomerular filtration pressure.
Interactions
• Diuretics synergize with the hypotensive action of ACE inhibitors by depleting Na+ and raising renin levels. In diuretic treated patients, the starting dose of ACE inhibitors should be low.
Hyperkalaemia can occur if K+ supplements/K+ sparing diuretics are given with any ACE inhibitor
Comparative features of ACE inhibitors
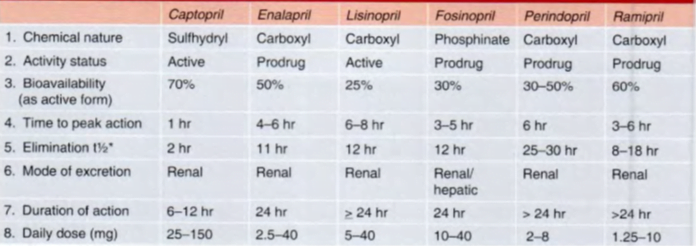
Enalapril
- prodrug. de-esterified in the liver to enalaprilat ànot used as such orally because of poor absorption à marketed as injectable preparation in some countries.
- Its absorption is not affected by food.
- It has a longer duration of action: most hypertensives can be treated with a single daily dose.
Captopril and lisinopril: only active, rest prodrug
Fosinopril
- unique in being a phosphinate compound that is glucuronide conjugated and eliminated both by liver and kidney. The t½ is not altered by renal impairment and the dose remains the same.
Ramipril
- extensive tissue distribution. Greater inhibition of local RAS has been claimed.
Quinapril
- Like ramiprilat, it is highly bound to the tissue ACE and exhibits a biphasic plasma t½ of 2 hours and 24 hours.
Perindopril à longest acting
USES
- Hypertension
- first-line drugs in all grades of hypertension, but the angiotensin receptor blockers (ARBs) have now surpassed them in popularity.
- About 50% of patients of essential hypertension respond to monotherapy with ACE inhibitors and many of the rest to their combination with diuretics or blockers.
- antihypertensive effect à lower doses develop gradually over 2- 3 weeks.
Advantages:
• Free of postural hypotension, electrolyte disturbances, feeling of weakness and CNS effects.
• Can be used in asthmatics, diabetics and peripheral vascular disease patients.
• Long-term therapy à potential to reduce incidence of type 2 diabetes in high-risk subjects.
• Secondary hyperaldosteronism and K+ loss due to diuretics is prevented.
• Renal blood flow is well maintained.
• Left ventricular hypertrophy and the increased wall-to-lumen ratio of blood vessels that occurs in hypertensive patients is reversed.
No hyperuricemia, no deleterious effect on plasma lipid profile.
• No rebound hypertension on withdrawal.
• Minimum worsening of quality of life parameters like general wellbeing, work performance, sleep, sexual performance, etc.
reduce cardiovascular morbidity and increase the life expectancy of hypertensive -> specific effect on myocardial and vascular cell growth/remodeling
first-choice drugs in renovascular and resistant hypertension -> particularly suitable for diabetic hypertensives in whom they reduce cardiovascular complications more than other antihypertensive drugs, probably by improving endothelial function.
- CHF
- both arteriolar and venodilatation in CHF patients;
- reduce afterload as well as preload on the heart and improve all hemodynamic parameters.
- stroke volume and cardiac output are increased, while the heart rate is reduced.
- Diuresis occurs initially and the accumulated salt and water are lost due to improved renal perfusion and abolition of mineralocorticoid mediated Na+ retention.
- Cardiac work = heart rate x pressure product is reduced;
- exercise capacity of CHF patients is enhanced.
- retard the progression of left ventricular systolic dysfunction and prolong the survival of CHF patients of all grades (I to IV).
- Mortality is reduced by ~ 20% in symptomatic CHF patients.
- ACE inhibitors reduce episodes of decompensation à reduce myocardial infarction and sudden death.
- improved hemodynamics, longterm benefits of ACE inhibitors à withdrawal of Ang II-mediated ventricular hypertrophy, remodeling, accelerated myocyte apoptosis and fibrosis.
- Myocardial infarction (Ml)
- Several megatrials have established that oral ACE inhibitors administered while Ml is evolving (within 24 hr of an attack) and continued for 6 weeks
- reduce early as well as long-term mortality,
- In unstable angina/non-ST segment elevation Ml ( STEMl), long-term ACE inhibitor therapy reduces recurrent MI and need for coronary angioplasty (SAVE and SOLVD trials)
- Prophylaxis in high cardiovascular risk subjects
- (HOPE) study in post-MI and other high-risk subjects, but having no left ventricular dysfunction or heart failure à ramipril reduced cardiac death and MI or stroke by 22% over a period of 4.5 years.
- The risk of developing heart failure or diabetes was also reduced.
- Thus, ACE inhibitors are protective in high cardiovascular risk subjects even when there is no associated hypertension or left ventricular dysfunction.
- Diabetic nephropathy
- Prolonged ACE inhibitor therapy has been found to prevent or delay the end-stage renal disease in type I as well as type II diabetics.
- Treated patients have higher creatinine clearance, require less dialysis and have a longer life expectancy.
- Reduce intraglomerular pressure and hypertiltration.
- All patients with diabetic nephropathy, whether hypertensive or normotensive, deserve ACE inhibitor therapy.
- These drugs reduce proteinuria by decreasing the pressure gradient across glomerular capillaries as well as by altering membrane permeability. This retards disease progression.
- Scleroderma crisis
The marked rise in BP and deterioration of renal function in scleroderma crisis is mediated by Ang II. ACE inhibitors produce dramatic improvement and are life-saving in this condition.
Captopril test: This test has been devised to obviate the need for renal angiography for diagnosis of renovascular hypertension. The basis of the test is-acute blockade of Ang II formation by captopril results in a reactive increase in PRA which is much higher in renovascular compared to essential hypertension. However, this test is only of adjunctive value.
C - Cough A - Angioedema P - Prodrugs (except captopril and Lisinopril) T - Taste disturbances O - Orthostatic hypotension (when combined with diuretics) P - Pregnancy (contra-indicated) R - bilateral Renal artery stenosis (contra-indicated) I - Increased K+(contra-indicated) L - Lower the formation of Ang Il (Mechanism)
ANGIOTENSIN ANTAGONISTS
(Angiotensin receptor blockers or ARBs)
losartan, candesartan, valsartan, telmisartan, olmesartan, and irbesartan, Eprosartan
- orally active AT1 receptor blockers
Losartan
- 10,000 times more selective for AT1 than for AT2 receptor
- does not block any other receptor or ion channel, except thromboxane A2 receptor (has some platelet antiaggregatory property).
- AII overt actions of Ang II, viz.
- vasoconstriction,
- central and peripheral sympathetic stimulation,
- release of aldosterone and Adrenaline from adrenals,
- renal actions promoting salt and water reabsorption,
- central actions like thirst, vasopressin release and
- growth-promoting actions on heart and blood vessels are blocked.
ARBs differ from ACE inhibitors in the following ways:
• do not interfere with the degradation of bradykinin and other ACE substrates: no rise in level or potentiation of bradykinin, substance P occurs àConsequently, ACE inhibitor-related cough is rare.
• result in more complete inhibition of AT1 receptor activation, because responses to Ang II generated via alternative pathways and consequent AT 1 receptor activation (which remain intact with ACE inhibitors) are also blocked.
• They result in indirect AT2 receptor activation. Due to blockade of AT I receptor-mediated feedback inhibition- more Ang II is produced which acts on AT2 receptors that remain unblocked.
• ARBs cause little increase in the level of Ang ( 1-7) which is raised by ACE inhibitors since Ang ( 1-7) is also partly degraded by ACE. The impact of these differences on clinical efficacy and therapeutic value of the two classes of RAS inhibitors is not known.
Adverse effects
- Like ACE inhibitors it can cause hypotension and hyperkalemia, but first dose hypotension is uncommon
- Though a few reports of dry cough have appeared à Patients with a history of ACE inhibitor-related cough have taken losartan without recurrence.
- Angioedema – fewer cases
- Headache, dizziness, weakness and upper g.i. side effects are mild and occasional.
- fetopathic potential like ACE inhibitors
Eprosartan
- newer AT1 receptor antagonist, shortest acting
- believed to lower BP by blocking vasoconstrictor AT1 receptors as well as by reducing NA release.
- Though blockade of prejunctional AT1 receptors on sympathetic neurons and the resultant decrease in sympathetic outflow is a class effect of ARBs, this action is claimed to be more prominent in eprosartan.
Telmisartan à longest acting, additional PPAR- gamma agonist activity, can help in patients with dysglycemia.
DIRECT RENlN INHIBITOR
Aliskiren, Remikiren, Enalkiren
- The latest class of RAS inhibitory drugs
- available for the treatment of cardiovascular and renal diseases in which ACE inhibitors and ARBs are currently used
- nonpeptide which binds selectively to the catalytic site of renin and competitively blocks the access or angiotensinogen to this site.
- As a result, Ang 1 is not produced and the effector chain of RAS is interrupted.
- While the concentration of renin in plasma is increased by feedback, the plasma renin activity (PRA) is decreased.
- Ang I and Ang II levels fall in a dose-dependent manner.
- Aliskiren causes dose-related fall in BP which is more marked in the depleted subject with high basal PRA.
- Similar to ACE inhibitors, plasma aldosterone levels are lowered accompanied by mild natriuresis and a tendency to K+ retention.
- Antihypertensive efficacy of aliskiren à nearly equivalent to that of ACE inhibitors or ARBs.
- A combination of these drugs with aliskiren produces greater fall in BP, at least in the short term. This is due to a blockade of the rise in PRA caused by ACE inhibitors/ARBs.
- postural hypotension is not a problem.
- Trials so far à it reduces hypertensive left ventricular hypertrophy and benefits CHF patients, but its value compared to ACE inhibitors/ARBs as monotherapy and as the additional drug remains to be established on the basis of outcome data.
- Aliskiren reduces albuminuria and has a renoprotective effect in hypertension and diabetes mellitus.
- At present, aliskiren is recommended as an alternative antihypertensive drug (for those who do not respond or do not tolerate I st line drugs) and in combination with ACE inhibitor/ARB to achieve more complete RAS blockade and greater BP lowering/cardioprotection.
- However, the addition of aliskiren to ACE inhibitor/ARB in type 2 diabetics has not produced any beneficial effect; it may even worsen outcome and is not advised.
- Plasma t½ is > 24 hours, and its BP-lowering effect persists for days after regular intake.
Adverse effects
mild side effects- mainly dyspepsia, abdominal pain, loose motions, headache, and dizziness. Acute hypotension, hyperkalemia, cough, angioedema, and rashes are less frequent than with ACE inhibitors.
Aliskiren is contraindicated during pregnancy.
JNC 8
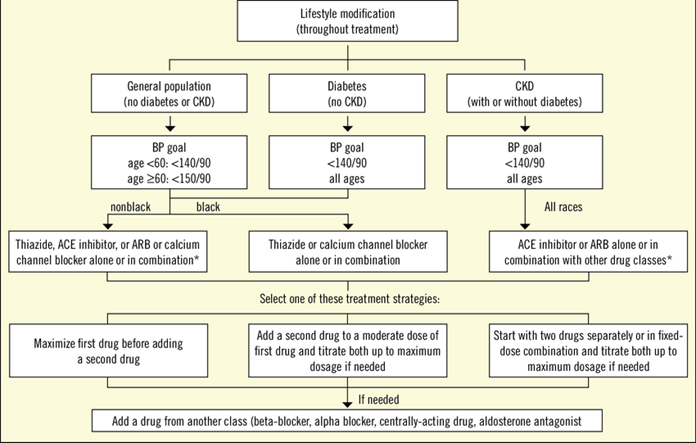
Beta blockers- no longer considered as 1st lineà due to increased mortality
Indian HTN guideline 2016
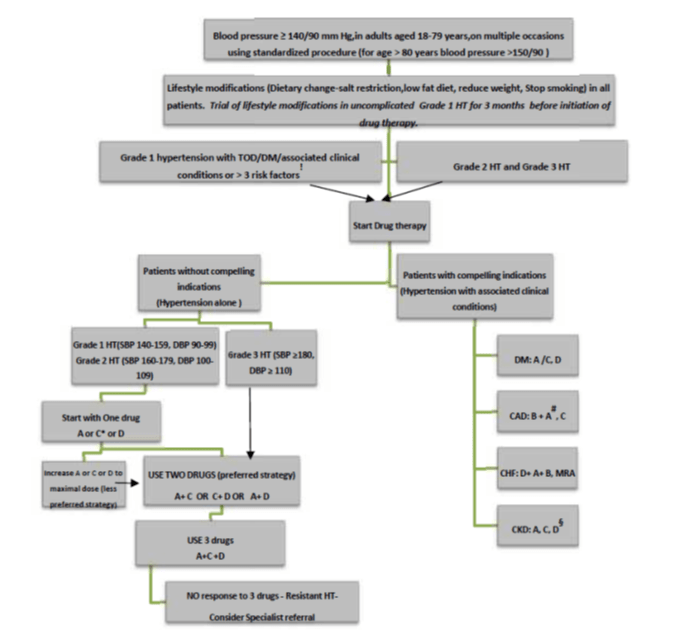
Drug abbreviations: A : Angiotensin-converting enzyme(ACE) inhibitors (e.g. enalapril) or Angiotensin II receptor blockers(ARBs)(e.g. losartan) only if intolerance to ACE inhibitors, C: Calcium channel blocker(e.g. amlodipine), D: Thiazide diuretics(e.g. hydrochlorothiazide), B: Beta-blockers(e.g. atenolol), MRA : Mineralocorticoid receptor antagonist (e.g. spironolactone).
