Bronchial Asthma
- Condition of bronchial hyperreactivity associated with inflammation.
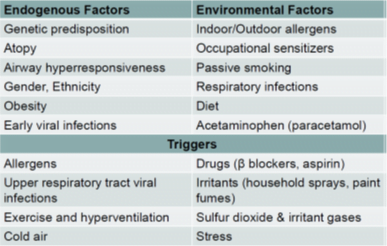
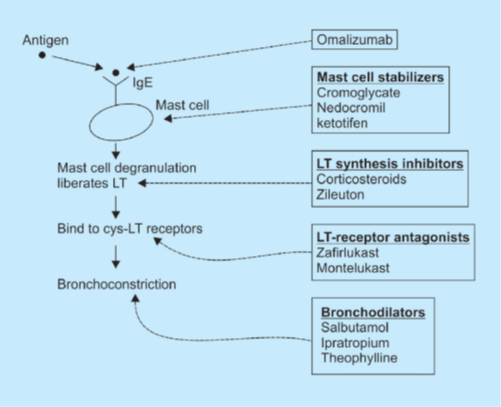
- IgE binds to mast cells on first exposure to antigen. On subsequent exposure, the antigen binds to this IgE (bound to mast cells) and its activation leads to degranulation of mast cells, resulting in the release of mediators.
- Important mediators include leukotrienes (LTs), prostaglandins (PGs), platelet-activating factor (PAF), histamine and protease enzymes.
- These mediators can lead to bronchoconstriction (and thus acute attack of asthma) as well as inflammation leading to hyperreactivity.
- The only drugs effective for the treatment of an acute attack of bronchial asthma are bronchodilators (sympathomimetics, parasympatholytics, and methylxanthines).
1. Bronchodilators
These are the only drugs useful in terminating acute attack of bronchial asthma. Three groups of drugs may act as bronchodilators:
Sympathomimetics
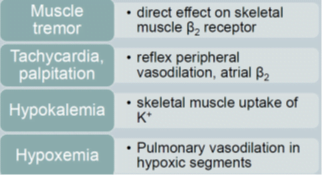
- Adrenergic drugs (β2 agonists) act by stimulating GPCRs that result in the activation of adenylyl cyclase and finally increase in cAMP, which causes smooth muscle relaxation (bronchodilation).
- cAMP also decreases the mediator release from mast cells.
- These drugs also inhibit microvascular leakage and increase mucociliary transport by increasing ciliary activity.
- By inhalational route, these are the fastest acting drugs.
- Adrenaline and isoprenaline produce bronchodilation quickly whereas ephedrine has a slower onset of action. Above mentioned drugs are non-selective and thus are not preferred (tachycardia and increase in the BP are their side effects).
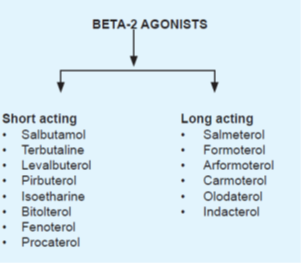
- Selective β2 agonists are preferred agents for bronchial asthma.
- Salbutamol, Levalbuterol, pirbuterol, terbutaline, isoetharine, bitolterol, fenoterol, and procaterol are short-acting whereas
- salmeterol, formoterol, arformoterol, carmoterol, olodaterol, and indacaterol are long-acting β2 agonists.
- Salbutamol (albuterol), metaproterenol, pirbuterol, and terbutaline are fast-acting drugs by inhalational route (optimal particle size: 2-5 μm, deposition can be increased by holding the breath in inspiration), so they are used for aborting an attack of acute asthma.
- These drugs are not suitable for prophylaxis because of a shorter duration of action.
- Chronic use of these drugs may lead to tolerance due to the downregulation of β2 receptors.
- Salmeterol, bambuterol (prodrug of terbutaline) and formoterol are long-acting β2 selective agonists.
- Salmeterol is delayed acting, therefore useful only for prophylaxis whereas formoterol is fast-acting also, so it is useful in aborting acute attack of bronchial asthma as well as for prophylaxis.
- Bitolterol is a prodrug and is activated to form colterol by esterases in the lung.
Adverse effects beta-blockers:
Anticholinergics
- cause dilation of mainly large airways (β2 agonists cause bronchiolar dilation).
- less efficacious and slower acting bronchodilators than sympathomimetics.
- more effective for COPD than bronchial asthma.
- Ipratropium, tiotropium, and umeclidinium are anticholinergic drugs (M3 antagonists) that can be used only by the inhalational route.
- Tiotropium and umeclidinium are longer acting than ipratropium.
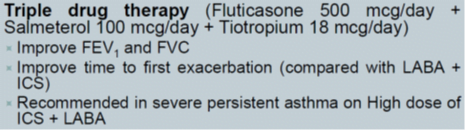
- Tiotropium is used in long-term prophylaxis of bronchial asthma (only in combination with corticosteroids)
- whereas umeclidinium is used for maintenance treatment of airflow obstruction in COPD.
- bronchodilators of choice in patients of bronchial asthma on β blocker therapy (β2 agonists will be ineffective).
Methylxanthines
- This group includes caffeine, theophylline, and theobromine.
- act by blockade of adenosine receptors (adenosine is a bronchoconstrictor) and by inhibition of enzyme phosphodiesterase (involved in the breakdown of cAMP).
- At a high dose, these drugs can result in the release of Ca++ from the sarcoplasmic reticulum in skeletal and cardiac muscles.
- These drugs are CNS stimulant drugs and at a toxic dose can result in tremors, delirium, and convulsions.
- These can lead to vomiting due to gastric irritation and CTZ stimulation.
- Theophylline is a potent vasodilator (due to an increase in cAMP) and can cause hypotension which leads to reflex tachycardia.
- Positive chronotropic and inotropic effects may be produced even at low doses due to inhibition of presynaptic adenosine receptors (heteroceptors at sympathetic nerve endings).
- At toxic doses, arrhythmias can be produced.
- Theophylline is given by oral route and aminophylline is administered by slow i.v. infusion.
- Kinetics of theophylline changes from first-order to zero order within the therapeutic dose range.
- It has a narrow therapeutic index.
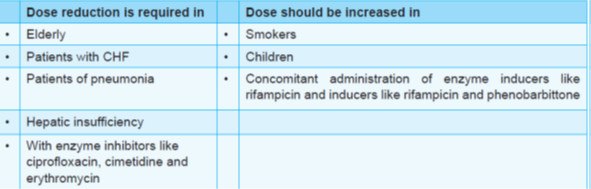
- Smoking and enzyme inducers (phenytoin, phenobarbitone, rifampicin, etc.) decrease the plasma levels of theophylline, therefore require an increase in dose.
- On the other hand, drugs like ciprofloxacin, erythromycin, and cimetidine are powerful microsomal enzyme inhibitors, predisposing to the toxicity of theophylline.
- Children clear theophylline faster than adults (require high dose) whereas clearance of theophylline is slower in elderly, premature infants and neonates (require less dose).
- Further, children are more liable to develop CNS toxicity.
Interactions of Theophylline
Apart from bronchial asthma, theophylline can also be used to reduce the frequency of episodes of apnea in premature infants because methylxanthines improve contractility and reverse fatigue of diaphragm.
Roflumilast, cilomilast and tofimilast are PDE-4 inhibitors being tried for bronchial asthma.
Recently, it has been found that theophylline at low doses exerts anti-inflammatory action by activating a nuclear enzyme; histone deacetylase-2.
Drug Inhibiting IgE Action
Omalizumab
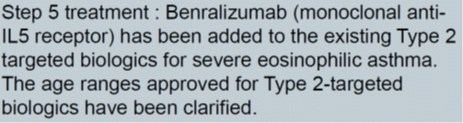
- monoclonal antibody against IgE and is indicated to prevent the attack of bronchial asthma in patients not responding to a combination of long-acting β2 agonists and a high dose of inhalational steroid.
- It is administered by s.c. route.
- Black box warning- anaphylaxis à patient should be observed for 2 hours after the first 3 injections and 30 mins after each subsequent dose.
Mast Cell Stabilizers
Sodium cromoglycate and nedocromil
- prevent the degranulation of mast cells by trigger stimuli.
- These are indicated only for prophylaxis of bronchial asthma.
- These are given by the inhalational route.
- Ketotifen has antihistaminic action apart from mast cell stabilizing the property and is specially indicated for patients with multiple disorders (atopic dermatitis, perennial rhinitis, conjunctivitis, etc.).
Drugs Decreasing the Action of LTs
- includes the drugs that interfere with the generation of LTs (corticosteroids and lipoxygenase inhibitors) and
- interfere with the action of LTs ( leukotriene receptor antagonists).
Corticosteroids
- potent anti-inflammatory drugs and also decrease bronchial hyperreactivity and mucosal edema.
- Anti-inflammatory action is due to decreased recruitment of inflammatory cells as well as decreased production of PGs and LTs.
- Arachidonic acid (AA) is released from the membrane phospholipids with the help of enzyme phospholipase A2 that is inhibited by corticosteroids.
- AA is converted to PG and TX by cyclooxygenase and to LT with the help of enzyme 5-lipooxygenase (5 LOX).
- Thus, these mediators are not generated when corticosteroid therapy is initiated.
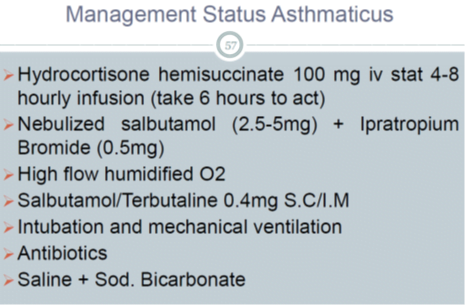
- Systemic steroids have a lot of adverse effects, therefore are reserved for resistant severe chronic asthma and in status asthmaticus.
- These are not bronchodilators but increase the sensitivity to β2 agonists.
- Inhaled steroids include beclomethasone, budesonide, mometasone, fluticasone, flunisolide, and triamcinolone.
- These have very little oral absorption and thus little systemic activity after inhalation (>90% reaches GIT after inhalational route, only 4-5% is retained in the lungs).
- Hoarseness of voice and oropharyngeal candidiasis are very common adverse effects.
- Candidiasis can be prevented by gargling after each dose and topical nystatin (can be used for treatment also).
- Systemic corticosteroids should be avoided in pregnancy but inhaled steroids are safe.
- Ciclesonide is an inhaled corticosteroid that is metabolized by enzymes in the lungs. Thus, it has the least risk of toxicity from systemic absorption when given inhalational. It is known as a soft steroid.
- Intramuscular triamcinolone acetonide is a depot preparation but proximal myopathy is a major problem with this therapy.
Lipooxygenase inhibitors
Zileuton
- inhibits the synthesis of LTB4 (chemotactic) and LTC4 and LTD4 (bronchoconstrictor).
- Limiting features of this drug are the short duration of action and hepatotoxicity.
LT receptor antagonists
- Montelukast and zafirlukast inhibit the bronchoconstrictor action of LTs at cys LT1 receptor.
- These are used as prophylactic agents for bronchial asthma.
- These are very safe drugs but few cases of Churg Strauss syndrome (vasculitis with eosinophilia) have been associated with their use.
Stepwise therapy of asthma
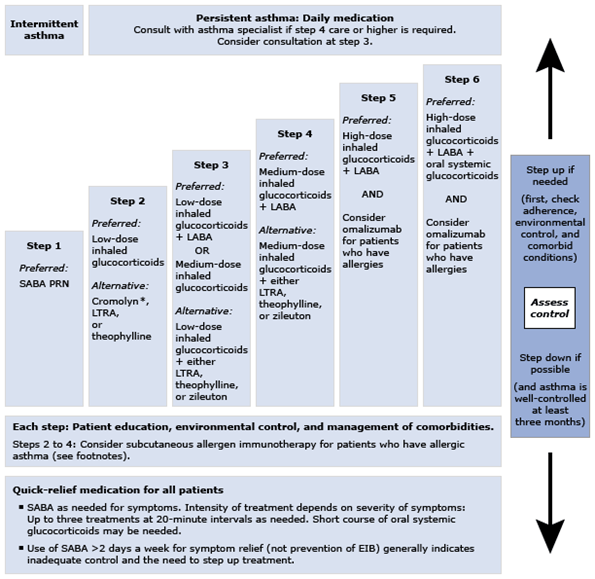
GINA 2018
• Exercise-Induced Asthma:
It typically begins after the end of exercise and recovers spontaneously within 30 minutes. Treatment is usually not required but can be done by SABA.
The best method to prevent exercise-induced asthma is regular treatment with inhaled corticosteroids (Ref. Harrison 17th/1601) which reduces mast cells.
Antileukotrienes, mast cell stabilizers, and β2 agonists can also be used for this function.
• Aspirin Induced Asthma:
Recently, it has been found that aspirin acetylated COX- 2 enzymes can convert arachidonic acid to 15-HETE (15-hydroxyeicosatetraenoic acid).
In WBCs, 15-HETE is converted to epi-lipoxins (15-epi-LXA4 or 15-epi LXB4).
These are called aspirin-triggered lipoxins and have powerful bronchoconstrictor action. This finding can explain the induction of asthma with aspirin but not by other COX-inhibitors.
Note:
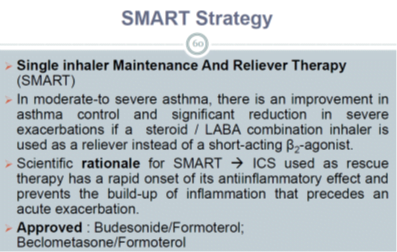
• LABA should not be given in the absence of ICS therapy as they do not control the underlying inflammation. Recently, the FDA has issued a black box warning for this combination due to a slightly increased risk of mortality from asthma attacks.
• In pregnancy; SABA, ICS and theophylline are considered safe.
Albuterol – preferred SABA
Budesonide – preferred ICS
If oral corticosteroids are required prednisone should be used. Because for action it needs to be converted to prednisolone and fetal liver cannot carry out this reaction.
The fetus is thus protected from the systemic effects of corticosteroids.
Respiratory System
Aerosol Delivery of Drugs
- Four classes of anti-asthma drugs (β2 agonists, anticholinergics, sodium cromoglycate, and steroids) can be administered by the inhalational route.
- This route is aimed to decrease the systemic side effects of these drugs.
- Two types of aerosols can be used.
• Aerosols using the drug in solution:
- These include metered-dose inhaler (MDI) and the nebulizer.
- MDI use chlorofluorocarbons (less preferred due to their effect on the ozone layer) or hydrofluoroalkane propellants.
- These deliver the drug in spray form.
- The disadvantage of these devices is that they require proper coordination between deep inspiration and inhaler activation which many patients (especially children and elderly) are unable to do.
- Use of a spacer decrease the requirement of this co-ordination
- Nebulizers produce a mist of drug solution generated by pressurized air.
- These do not require hand-inspiration co-ordination and are therefore preferred in children, elderly and very severe episodes of asthma.
• Aerosols using drugs as dry powder:
- These include spinhaler and rotahaler.
- The disadvantage of these devices is that they require +high-velocity inspiration (not suitable for children, elderly and very sick patients) and
- these can cause irritation of the air passage (leading to cough and bronchoconstriction).
