Emergency (postcoital) pill
- These are for use in a woman not taking any contraceptive who had a sexual intercourse risking unwanted pregnancy.
- reserved for unexpected or accidental exposure (rape, condom rupture) only, because all emergency regimens have higher failure rate and side effects than regular low-dose combined pill.
- There are no medical contraindications to use of oral emergency contraception.
- Neither a physical examination nor laboratory testing is needed before prescribing levonorgestrel or an estrogen-progestin regimen for emergency contraception
- Pregnancy should be excluded and, if not conclusively excluded by history, pregnancy testing should be performed, particularly before prescribing ulipristal or intrauterine contraception.
The most commonly used and standard regimen is-
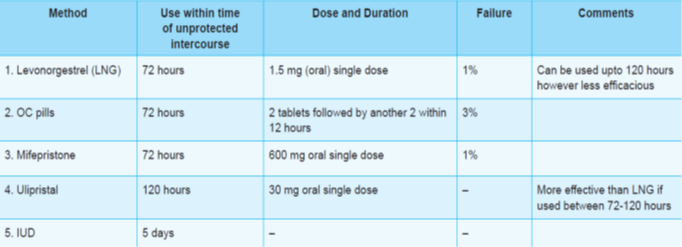
- Levonorgestrel 0.75 mg two doses 12 hours apart, or 1.5 mg single dose taken as soon as possible, but before 72 hours of unprotected intercourse.
- Trials conducted globally by a WHO task force on postovulatory methods of fertility control have found this regimen to be 2-3 times more effective and better tolerated than the earlier ‘Yuzpe method‘ which used levonorgestrel 0.5 mg + ethinyl estradiol 0.1 mg, two doses at 12 hours interval within 72 hours of exposure.
- Incidence of nausea and vomiting is nearly 6% in the progestin only regimen compared to 20-50% with the estrogen + progestin regimen.
- Headache and other side effects are also milder.
- However, the next period may be delayed or disrupted with either regimens.
- Ulipristal
- selective progesterone receptor modulator with primarily antiprogestin activity.
- 30 mg single dose as soon as possible, but within 120 hours of intercourse.
- equally effective (failure rate 1- 3% compared to levonorgestrel 2- 4%) and
- equally well tolerated alternative method now available with an extended window of protective action
- Their primary mechanism of action is delay of ovulation, but endometrial effects that may affect implantation may also contribute to efficacy
- disadvantage of antiprogestins is that the delay in ovulation results in a delay in subsequent menses, which may provoke anxiety about possible pregnancy
- Another anti-progestin à used particularly in Europe and China à Mifepristone 600 mg single dose taken within 72 hours of intercourse.
- Copper intrauterine contraception inhibits fertilization by affecting sperm viability and function. The copper device also has postfertilization contraceptive effects
- Copper intrauterine contraception (IUD) is the most effective method of emergency contraception
- Advantages of this method are that it provides continuing contraception after initial IUD placement, is more effective than oral regimens, especially in overweight/obese women, and is well tolerated, with one-year continuation rates of 60 percent
Repeated emergency contraception —
There is no contraindication to giving a second dose of hormonal emergency contraception if a second episode of unprotected intercourse occurs any time after the first dose was administered
Investigational drugs:
- Prostaglandin inhibitors — Drugs of this class (COX-1 and COX-2 inhibitors) appear to interfere with several essential steps in female reproduction, including oocyte maturation and ovulation.
- Meloxicam — In a study of 41 women with leading follicles ≥15 mm, treatment with meloxicam (15 mg) plus levonorgestrel (1.5 mg) resulted in a significantly higher proportion of cycles with no follicular rupture within five days than treatment with placebo plus levonorgestrel (88 versus 66 percent of cycles)
