Immunomodulators
- Immunity is usually defined as a state of relative resistance to an infection.
- Components of immune system:
- Lymphocytes
- Cellular immunity
- Humoral immunity
- Immunoglobulin
- Lymph nodes
- Spleen
- Thymus
- There are 2 types of immunity:
- Active immunity.
- Passive immunity.
The important components of immune system include:
- Granulocytes
- Complement synthesis & antibody formation
- Cellular immunity
- Mucocutaneous barriers
Mechanisms of immunomodulation
- Drugs may modulate immune mechanism by either suppressing or by stimulating one or more of the following steps:
- Antigen recognition & phagocytosis
- Lymphocyte proliferation/differentiation
- Synthesis of antibodies
- Ag –Ab interaction
- Release of mediators due to immune response
- Modification of target tissue response
- The importance of immune system in protecting the body against harmful molecules is well recognized
- However, in some instances, this protection can result in serious problems
- E.g, the introduction of allograft can elicit a damaging immune response causing rejection of the transplanted tissue
- Benefits of immunomodulators stem from their ability to stimulate natural & adaptive defence mechanisms, such as cytokines, which enables the body to help itself
- Natural immunomodulators act to strengthen weak immune systems & to moderate immune systems that are overactive
- Plant sterols & sterolins are natural immunomodulators found in some raw fruits & vegetables & in the alga, spirulina
- Immunomodulators: “These are the drugs which alters the immune system in a way such as to suppress it (immunosuppressants ) or enhance it (immunostimulants).
| Phases of immune response | Suppressants | Enhancers |
| Antigen recognition & processing | Corticosteroids Cyclophosphamide | BCG vaccine Tetramisole |
| Amplification | L- Asparaginase Corticosteroids Cyclophosphamide 5-fluorouracil | Concanavalin A Tetramisole |
| Antibody formation | Corticosteroids Cyclophosphamide Cyclosporin A | Lipopolysaccaride Tetramisole |
| Immune affector response | Corticosteroids Cylcophosphamide Cyclosporin A Methotrexate | Tetramisole |
Immunomodulators types
- All drugs which modify immune response generally categorized as immunomodulators. These can either function as:
- 1. Immunosuppressants
- 2. Immunostimulants
- Some of these can have both the properties depending on which component of immune response they affect
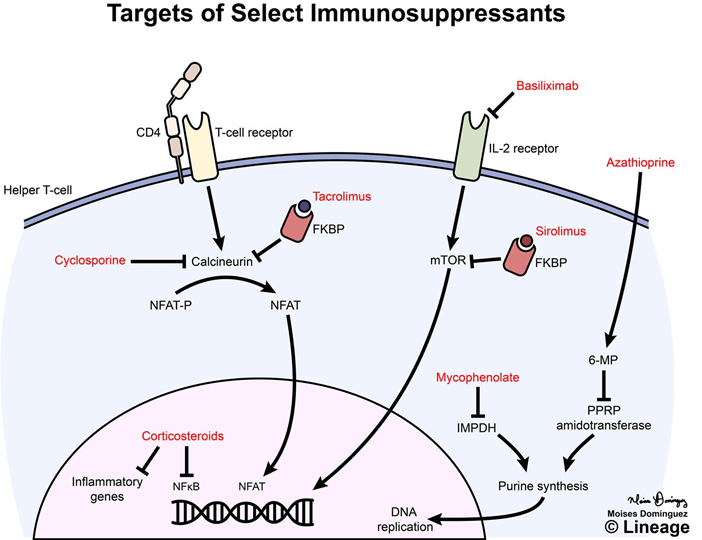
Immunosuppressants
- Glucocorticoids
- Calcineurin inhibitors
- Cyclosporine
- Tacrolimus
- Antiproliferative / antimetabolic agents
- Sirolimus
- Everolimus
- Azathioprine
- Mycophenolate Mofetil
- Others – methotrexate, cyclophosphamide, thalidomide & chlorambucil
- Antibodies
- Anti-thymocyte globulin
- Anti CD3 monoclonal antibody
- Muromonab
- Anti IL-2 receptor antibody –
- Daclizumab, basiliximab
- Anti TNF alpha – infliximab, etanercept, Adalimumab.
- Immunosuppressants are the drugs which inhibit cellular/humoral or both types of immune responses, & have their major use in organ transplantation & autoimmune disease
- Problems arising – Life-long use
Infection, cancers
Nephrotoxicity
Diabetogenic
Glucocorticoids
- Induce redistribution of lymphocytes – decrease in peripheral blood lymphocyte counts
- Down regulation of IL-1, IL-2, IL-3, IL-6
- Inhibition of T cell proliferation
- Increase number of RBCs, platelets & neutrophils in circulation
- Enhance rate of destruction of lymphoid cells
Uses
- Transplant rejection
- GVH – BM transplantation
- Autoimmune diseases – RA, SLE, Hematological conditions
- Psoriasis
- Inflammatory Bowel Disease, Eye conditions
Toxicity
- Growth retardation
- Avascular Necrosis of Bone
- Risk of Infection
- Poor wound healing
- Cataract
- Hyperglycemia
- Hypertension
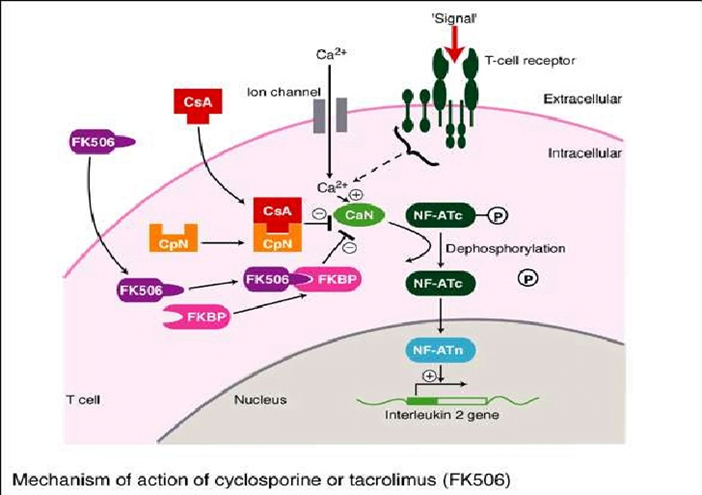
Calcineurin inhibitors
- Cyclosporine &Tacrolimus
- Most effective immunosuppressive drugs
- Target intracellular signaling pathways
- Blocks Induction of cytokine genes
Cyclosporine
- Cyclic peptide composed of 11 amino acid
- Extracted from a soil fungus
- Selectively inhibits T lymphocyte proliferation, IL-2 & other cytokine production & response of inducer T cells to IL-1, without any effect on suppressor T cells
- Lymphocytes are arrested at G0 or G1 phase
- Binds to the cytosolic protein cyclophilin (immunophilin) of immunocompetent lymphocytes, especially T-lymphocytes
- This complex of cyclosporine & cyclophilin inhibit calcineurin, which, under normal circumstances, is responsible for activating the transcription of IL-2
- It also inhibits lymphokine production & IL release, leads to a reduced function of effector T-cells, does not affect cytostatic activity
- Topical cyclosporine ophthalmic emulsion 0.05%
- Currently the only pharmacologic treatment that is FDA approved (2003) specifically for DED (Dry Eye Disease).
- Indicated to increase tear production in patients whose tear production is presumed to be suppressed due to ocular inflammation associated with keratoconjunctivitis sicca.
- Inhaled cyclosporine is being investigated for use in lung transplantation.
Uses:
- Prevent rejection of kidney, liver, cardiac, BM & other allogeneic transplants
- Can be used alone
- More effective when glucocorticoids are also administered
- Most active when administered before antigen exposure
- Useful in autoimmune disease as well
- Alternative to methotrexate for the treatment of severe, active RA
- Selectively suppresses CMI
- Free of toxic effects on BM & RE system
- For induction it is started orally 12 hrs before the transplant & continued for as long as needed
- When graft rejection has started, it can be given i.v
- Concentrated in RBCs & WBCs
- Metabolized in liver excreted in bile
- Biphasic t1/2: 4 -6hrs & 12 -18hrs

Toxicity : Cyclosporine
- Renal dysfunction
- Tremor
- Hirsutism
- Hypertension
- Hyperlipidemia
- Gum hyperplasia
- Hyperuricemia – worsens gout
- Calcineurin inhibitors + Glucocorticoids = Diabetogenic
Tacrolimus (FK506)
- Chemically different from cyclosporine, newer immunosuppressant
- Macrolide that is isolated from soil fungus
- Binds to different cytoplasmic immunophilin protein labelled FK506 binding protein(FKBP)
- Same MOA, 100 times more potent
- Orally as well as i.v infusion
- Metabolized by CYP3A4 & excreted in bile & plasma t1/2 is 12hrs
- Clinical efficacy as well as toxicity profile are similar to cyclosporine
- Tacrolimus 0.03% and 0.1% ointment – FDA approved in Dec. 2000.
- Pimecrolimus 1% cream – FDA approved in Dec. 2001.
- Indication: second-line therapy for the short-term and non-continuous chronic treatment of moderate to severe atopic dermatitis in non immunocompromised adults and children.
- Not to be used in children less than 2 years.
- ADR: burning, pruritus, erythema, edema, increased incidence of malignancies.
On February 2005, the FDA issued a warning on the potential risk of neoplasms following the topical application of Calcineurin inhibitors
Toxicity – Tacrolimus
- Nephrotoxicity
- Neurotoxicity-Tremor, headache, motor disturbances, seizures
- GI Complaints
- Hypertension
- Hyperglycemia
- Risk of tumors, infections
- Drug interaction
- Synergistic nephrotoxicity with cyclosporine
- CYP3A4
Sirolimus
- Macrolide antibiotic
- Binds to same immunoglobulin FKBP as Tacrolimus
- Sirolimus-FKBP complex inhibits another kinase called ‘mammalian target of rapamycin (mTOR) (does not interact with calcineurin)
- Leads to proliferation & differentiation of T-cells activated by IL-2
- Extensively metabolized mainly by CYP3A4
- Elimination primarily by biliary route
- T1/2- approx 60 hours
Uses
- Prophylaxis of organ transplant rejection along with other drugs (cyclosporin/tacrolimus)
Toxicity
- Increase in serum cholesterol, Triglycerides
- Anemia
- Thrombocytopenia
- Hypokalemia
- Fever
- GI effects
- Risk of infection, tumors
Sirolimus – eluting coronary stent
- FDA approved in April 2003.
- Sirolimus drug-eluting stents have been shown to reduce restenosis without increasing the risk of stent thrombosis in comparison with bare metal stents through their inhibitory actions on vascular smooth muscle cell proliferation.
Everolimus
- Similar to sirolimus in mechanism, clinical efficacy, doses & drug interactions
- Better absorbed orally
- Shorter half life (approx 40 hours)
- Shorter time taken to reach steady state
- Similar uses & toxicity
- Everolimus-eluting stents have recently become available in the USA and Europe.
Temsirolimus
- More water-soluble ester of rapamycin.
- Available in both i.v. and oral formulations.
- S/Es – asthenia, mucositis, nausea and cutaneous toxicity.
- Approved by FDA in 2007 for advanced Renal Cell Carcinoma (RCC).
Azathioprine
- Purine antimetabolite
- Selectively affects differentiation & function of T-cells
- Inhibits cytolytic T-lymphocytes, CMI is primarily depressed
Uses
- Prevention of renal & other graft rejections
- Rheumatoid arthritis(lower doses)
Toxicity
- Bone marrow suppression- leukopenia, thrombocytopenia, anemia
- Increased susceptibility to infection
- Hepatotoxicity
- Alopecia
- GI toxicity
- Drug interaction: Allopurinol
Mycophenolate Mofetil
- Newer immunosupressant
- Prodrug of Mycophenolic acid
- Inhibits Inosine Monophosphate Dehydrogenase – enzyme in guanine synthesis
- Inhibits lymphocyte proliferation, antibody production & CMI
Uses:
- Prophylaxis of renal transplant rejection
- Mycophenolate mofetil+ glucocorticoid + sirolimus – non-nephrotoxic combination utilized in patients developing renal toxicity with cyclosporin/tacrolimus
Toxicity
- GI, Hematological
- Diarrhea, Leucopenia
- Risk of Infection(CMV infections)
Cyclophosphomide
- More marked effect on B cells & humoral immunity
- Used in BM transplantation in which short course with high dose is given
- In other organ transplantations it is employed only as a reserve drug
- In RA, it is rarely used
- Low doses are occasionally employed for maintenance therapy in pemphigus, SLE & idiopathic thrombocytopenic purpura
Methotrexate
- Folate antagonist, potent immunosupressant
- Markedly depresses cytokine production & cellular immunity & has anti-inflammatory property
- Used as 1st line drug in many autoimmune diseases like rapidly progressing RA, severe psoriasis, pemphigus, myasthenia gravis, uveitis, chronic active hepatitis
- Low dose as maintenance therapy is relatively well tolerated
Fingolimod
- Sphingosine 1 Phosphate Receptor agonist
- Reduce recirculation of lymphocytes from lymphatic system to blood & peripheral tissues
- “Lymphocyte homing” – periphery into lymph node
- Protects graft from T-cell-mediated attack
Uses
- Combination immunosuppression therapy in prevention of acute graft rejection
Anti-thymocyte Globulin
- Polyclonal antibody purified from horse or rabbits immunized with human thymic lymphocytes
- Binds to T lymphocytes & depletes them
- Potent immunosupressant
Uses
- Induction of immunosuppression – transplantation
- To suppress acute allograft rejection episodes
Toxicity
- Hypersensitivity
- Risk of infection, Malignancy
Anti-CD3 Monoclonal Antibody
- Murine monoclonal antibody against the CD3 glycoprotein expressed near to the T cell receptor on helper T cell
- Binds to CD3, a component of T-cell receptor complex involved in
- antigen recognition
- cell signaling & proliferation
Muromonab
Antibody treatment àRapid internalization of T-cell receptor à Rapid T-cell depletion from blood
à Prevents subsequent antigen recognition
Use
- Treatment of acute organ transplant rejection
Toxicity
- “Cytokine release syndrome”
- Aseptic meningitis, life threatening pulmonary edema(rare)
Anti-IL-2 Receptor Antibodies
- Daclizumab & Basiliximab
- Bind to IL-2 receptor with high affinity on surface of activated T cells à Block IL-2 mediated T-cell activation
Uses
- Prophylaxis of Acute organ rejection & maintenance of graft
Toxicity
- Anaphylaxis, Opportunistic Infections
Campath-1H (Alemtuzumab)
- Monoclonal antibody binds CD52 – expressed on lymphocytes, monocytes, macrophages
- Extensive lympholysis – Prolonged T & B cell depletion
Uses
- CLL, Bone marrow transplantation, Renal transplantation
Toxicity
- Opportunistic infections
Anti-TNF Agents
- TNF – Cytokine at site of inflammation
- Infliximab
- Etanercept
- Adalimumab
Etanercept
- Fusion protein
- Ligand binding portion of Human TNF-α receptor fused to Fc portion of human IgG1
- Neutralizes both TNFα & TNFß
- Prevents activation of macrophages & T-cells
Uses
- Rheumatoid arthritis
- Also approved for severe/refractory ankylosing spondylitis, plaque
Infliximab
- Chimeric monoclonal antibody against TNFα
Uses
- Rheumatoid arthritis
- Chron’s disease – fistulae
- Psoriasis
- Psoriatic arthritis
- Ankylosing spondylosis
Toxicity
- Infusion reaction – fever, urticaria, hypotension, dyspnoea
- Opportunistic infections – TB, RTI, UTI
Immunostimulants
- Levamisole
- Thalidomide
- BCG
- Recombinant Cytokines
- Interferons
- Interleukin-2
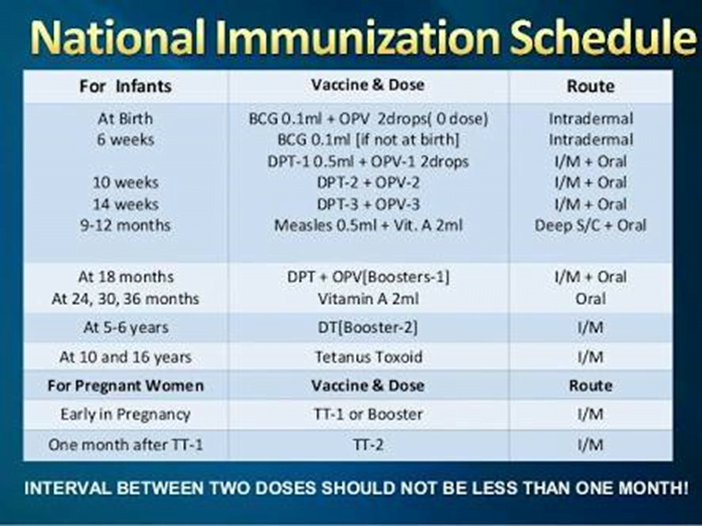
Immunization
- Vaccines
- Immune Globulin
- Rho (D) Immune Globulin
TETRAMISOLE (LEVAMISOLE)
- An anthelminthic drug.
- Levamisole is orally active levo-isomer of tetramisole, restores depressed T-cell function
- Used as an adjunct in malignancies, aphthous ulcers & recurrent herpes, also used as disease modifying drug in Rheumatoid Arthritis
- Mainly acts by raising c-GMP levels through interaction with thymopoietien receptor sites
- leads to decrease in metabolic inactivation of c-GMP accompanied with increased breakdown of c-AMP
- Increase in c-GMP level induces lymphocyte proliferation & augmentation of chemotactic responses
- This reflects into increased antibody production, lymphokine production, increased phagocytosis
Thalidomide
- Anxiolytic, antiemetic drug with anti-inflammatory, cytokine modulatory activity
- Enhanced T-cell production of cytokines – IL-2, IFN-γ
- NK cell-mediated cytotoxicity against tumor cells
USE:
- Multiple myeloma, ENL
Lenalidomide – FDA approved in 2005.
- More potent, less toxic.
- Indication
- Myelodysplastic syndrome with the chromosome 5q31 deletion.
- In combination with dexamethasone for the treatment of multiple myeloma patients.
Bacillus Calmate Guerin (BCG) Vaccine
- It is used as immunological enhancer to stimulate intact immune system (i.e. a non-specific immune-enhancer) of the body.
- BCG & its methanol extracted residue (MER) contain muramyl dipeptide as an active immunostimulant ingredient
- T-lymphocytes are principle target cells for the action of BCG vaccine.
- It causes stimulation of macrophage function, phagocytic activity, lysosomal enzyme activity & chemotaxis mechanisms
- It induces the production of lymphocyte-activity factor resulting of phase I of immune response.
- Because of its activity against tumour antigen it is beneficial in treatment of lung & breast cancer, acute lympholytic & myelogeneous leukaemia.
- It is available as unlyophilized, live or killed lyophilized form.
Interferons
- Low molecular weight glycoprotein cytokines produced by host cells in response to viral infections
- Immunomodulatory activity
- Bind to cell surface receptors – initiate intracellular events
- Enzyme induction
- Inhibition of cell proliferation
- Affect viral replication
- Increased Phagocytosis
Interferon alfa-2b
- Hairy cell leukemia
- Malignant melanoma
- Kaposi sarcoma
- Chronic Hepatitis B
Adverse reactions
- Flu-like symptoms – fever, malaise, headache
- CVS- hypotension, Arrhythmia
- CNS- depression, altered behavior
Interferon gamma-1b
- Indication
- to reduce the frequency and severity of serious infections associated with chronic granulomatous disease.
- S/E – fever, headache, rash, fatigue, GI distress, anorexia, weight loss, myalgia, and depression.
Interferon beta-1a and interferon beta-1b
Indication
- Treatment of relapsing and relapsing-remitting multiple sclerosis to reduce the frequency of clinical exacerbations.
- S/E – Flu-like symptoms (fever, chills, myalgia) and injection-site reactions.
Interleukin-2 (aldesleukin)
- Human recombinant interleukin-2.
- Proliferation of cellular immunity – Lymphocytosis, eosinophilia, release of multiple cytokines – TNF, IL-1, IFN-γ
- Promotes differentiation of T-cells
Uses
- Metastatic renal cell carcinoma
- Malignant Melanoma
Toxicity
- Flu- like symptoms- fever, headache, fatigue
- Hypotension, drowsiness, confusion, loss of appetite
Imiquimod
- Interact with Toll like receptor TLR7 & TLR8 to boost innate immunity, including the secretion of interferons.
Approved for the t/t of certain diseases caused by HPVs
Oprelvekin
- Recombinant human IL -11.
- Prevention of thrombocytopenia in patient receiving highly myelosuppressive chemotherapy.
- S/E – Fatigue, fluid retention, Atrial fibrillation.
| Palivizumab | in RSV infections in children |
Active immunization
Vaccines
- Impart active immunity
- Active immunization more efficacious & longer lasting than passive immunization
- Booster doses required at certain intervals
- Anticancer vaccines – immunizing patients with APCs expressing tumor antigen
Immune Globulin
Indications
- Individual is deficient in antibodies – immunodeficiency
- Individual is exposed to an agent, inadequate time for active immunization
- Rabies
- Hepatitis B
- Nonspecific immunoglobulins
- Antibody-deficiency disorders
- Specific immune globulins
- High titers of desired antibody
- Hepatitis B, Rabies, Tetanus
Rho (D) Immune Globulin
- Antibodies against Rh(D) antigen on the surface of RBC
- Binds the Rho antigens & does not allow them to induce antibody formation in Rh –ve individuals
- Used for prevention of postpartum/post-abortion formation of antibodies in Rho-D –ve women (Hemolytic disease of newborn)
- Given at 28th week of pregnancy
Plants with immunostimulant potential
- Tinospora cordifolia
- Asparagus racemosus
- Phyllanthus emblica
- Withania somnifera
- Piper longum
- Terminalia chebula
- Aloe vera
