Medical treatment of benign prostatic hyperplasia
Prostatic enlargement with increased age is correlated with smooth muscle hyperplasia and may eventually lead to bladder outlet obstruction (BOO).
The most common presentation of subjective BPH-associated symptoms is lower urinary tract symptoms (LUTS).
LUTS may further be classified
- as obstructive symptoms: urine hesitancy, straining, weak flow, prolonged voiding, partial or complete urinary retention, and urinary incontinence.
- irritative symptoms: urinary frequency, urgency, nocturia, dysuria, and decreased void volume.
General Considerations
Behavioral interventions —
In patients with symptoms of (BPH) who do not have any discomfort and have no evidence of complications (such as bladder outlet obstruction, renal insufficiency, or recurrent infection), pharmacologic treatment may not be necessary.
These patients may be monitored and advised regarding behavioral modification.
Behavioral modification may be helpful for all patients.
- voiding in the sitting position (rather than standing)
- Avoiding fluids prior to bedtime or before going out
- Reducing consumption of mild diuretics such as caffeine and alcohol
- Double voiding to empty the bladder more completely
In one randomized trial, men given an educational intervention that included the teaching of behavioral modifications were significantly less likely to experience treatment failure (increase in International Prostate Symptom Score [IPSS] or requirement for medication) compared with men who chose watchful waiting alone
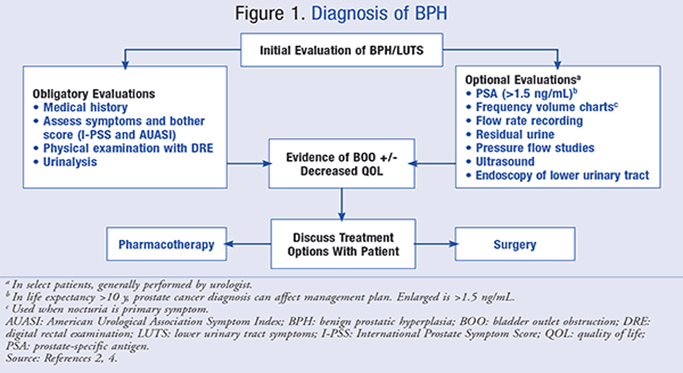
Indications for medical treatment —
The decision to medically à balances the severity of the patient’s symptoms with the potential side effects of therapy.
Unless patients have developed bladder outlet obstruction, BPH only requires therapy if symptoms have a significant impact on a patient’s quality of life
In addition to bladder outlet obstruction, there are several other situations in which patients should be referred to a urologist for evaluation prior to the initiation of medical therapy:
●Symptoms in the setting of autonomic or severe peripheral neuropathy
●Symptoms following invasive treatment of the urethra or prostate
●Men <45 years old
●Abnormality on the prostate exam (nodule, induration, or asymmetry)
●Presence of hematuria in the absence of infection
●Men with incontinence
●Severe symptoms (IPSS ≥20)
Overview —
In patients with mild (International Prostate Symptom Score [IPSS] <8) to moderate (IPSS 8-19) symptoms of BPH, we suggest initial treatment with an alpha-1-adrenergic antagonist monotherapy
Alpha-1-adrenergic antagonists provide immediate therapeutic benefits, while
5-alpha-reductase inhibitors require long-term treatment for efficacy.
Patients who experience side effects, such as hypotension, with alpha-1-adrenergic antagonists but still desire medical therapy for their BPH can be switched to 5-alpha-reductase inhibitors for monotherapy.
Treatment with 5-alpha-reductase inhibitors requires 6 to 12 months before symptom improvement.
Alternative options are available in specific populations of patients. Anticholinergic agents can be used in men who have predominately irritant symptoms, and
Phosphodiesterase-5 inhibitors are an option in men who also have erectile dysfunction.
In men with severe symptoms (IPSS ≥20), it may be reasonable to initiate therapy with a combination of an alpha-1-adrenergic antagonist and a 5-alpha-reductase inhibitor.
Medical management of BPH should be individualized based upon the nature and severity of symptoms and drug side effect profiles.
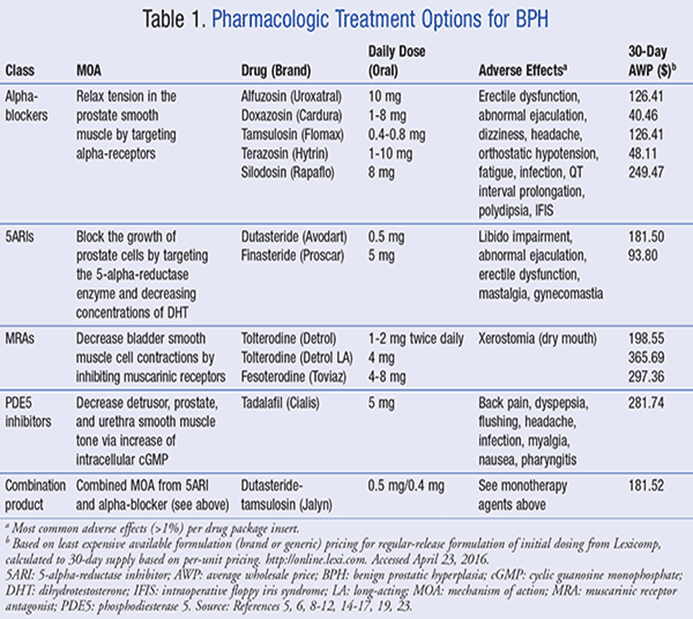
Alpha-1-adrenergic antagonists —
- for initial therapy of symptomatic BPH in most patients.
- act against the dynamic component of bladder outlet obstruction by relaxing smooth muscle in the bladder neck, prostate capsule, and prostatic urethra.
- Terazosin, doxazosin, tamsulosin, alfuzosin, and silodosin are long-acting alpha-1-antagonists à approved by the US Food and Drug Administration (FDA)
- Efficacy and administration —
Alpha-1-adrenergic antagonists appear to be more effective than 5-alpha-reductase inhibitors for short- and long-term treatment of BPH.
In a 2010 meta-analysis comparing alpha-adrenergic antagonist monotherapy versus finasteride (a 5-alpha-reductase inhibitor), doxazosin and terazosin were more effective in improving urinary symptoms compared with finasteride
Tamsulosin and finasteride were equally effective.
terazosin, doxazosin, tamsulosin, alfuzosin, and silodosin: similar efficacy, although there have been few direct comparisons
According to a 2017 meta-analysis, newer drugs à silodosin àassociated with similar short-term symptom reduction but the greater risk for adverse events (silodosin versus tamsulosin). Sexual side effects may be more common with silodosin compared with other drugs
- the choice of an agent may be based on cost, side effects (particularly hypotension), and potential medication interactions (especially with phosphodiesterase-5 inhibitors).
- Prazosin, a short-acting alpha-1-antagonist, is generally not used for BPH due to the need for frequent dosing and the potential for more cardiovascular side effects.
- Generally, it needs to be initiated at bedtime (to reduce postural lightheadedness soon after starting the medication), and the dose should be titrated up over several weeks.
Side effects and interactions —
●Hypotension – the most important side effects are orthostatic hypotension and dizziness.
Tamsulosin, alfuzosin, and silodosin have a lower potential to cause hypotension and syncope than either terazosin or doxazosin.
These differential effects on blood pressure by different alpha-1-antagonists may be due to their differential blocking of alpha-1 adrenoceptor subtype
●Interaction with phosphodiesterase-5 inhibitors – The hypotensive effects of terazosin and doxazosin can be potentiated by concomitant use of the phosphodiesterase (PDE)-5 inhibitors sildenafil or vardenafil.
●Ejaculatory dysfunction – Tamsulosin and silodosin, in particular, can affect ejaculation
Silodosin produces retrograde ejaculation in approximately 28 percent of patients
●Other side effects – Other common side effects include headache, dizziness, and nasal congestion.
Alpha-1-adrenergic antagonist use has also been associated with intraoperative floppy iris syndrome during cataract surgery.
5-alpha-reductase inhibitors —
In patients who desire medical therapy but cannot tolerate alpha-1-adrenergic antagonists and do not have predominately irritant symptoms or concomitant erectile dysfunction, treatment with a 5-alpha-reductase inhibitor is reasonable.
6 to 12 months is generally needed before prostate size is sufficiently reduced to improve symptoms.
5-alpha-reductase inhibitors are more effective in men with larger prostates.
MOA à act by reducing the size of the prostate gland and have demonstrated the potential for a long-term reduction in prostate volume and the need for prostate surgery.
The type 2 form of 5-alpha-reductase catalyzes the conversion of testosterone to dihydrotestosterone in the prostate, hair follicles, and other androgen-sensitive tissues.
Efficacy —
two 5-alpha-reductase inhibitors approved in the United States and Europe, finasteride and dutasteride.
Finasteride –
- efficacy of finasteride appears to persist with long-term treatment.
- improvements in symptom scores, maximal urinary flow rates, and prostate volume
- decreased the probability of surgery and acute urinary retention
- may also suppress gross hematuria that can occur in BPH
Dutasteride –
- improved symptom score and maximum flow rate while decreasing prostate volume, episodes of acute urinary retention, and need for surgical intervention
- The major side effect à sexual dysfunction.
Administration —
- Finasteride can be initiated and maintained at 5 mg once daily.
- Dutasteride can be initiated and maintained at 0.5 mg once daily.
- In contrast to the alpha-1-adrenergic antagonists, 5-alpha-reductase inhibitors do not require titration.
Side effects
●Concern regarding prostate cancer –Because of this concern, however, the FDA recommends that, before starting 5-alpha-reductase inhibitors for the treatment of BPH, the patient should be assessed for other urological conditions, including prostate cancer
Prior to starting any treatment for BPH, we evaluate patients with a digital rectal exam (DRE) and a serum prostate-specific antigen (PSA)
monitor annually with a DRE and a PSA.
●Sexual dysfunction – The major side effects à decreased libido and ejaculatory or erectile dysfunction
A meta-analysis found that the risk of ejaculatory dysfunction was similar to finasteride and dutasteride
●Prostate-specific antigen – PSA concentrations may decrease with 5-alpha-reductase inhibitor treatment. If a patient is being screened for prostate cancer, medication effect from 5-alpha-reductase inhibitors should be taken into account when interpreting the PSA.
●Depression – There have been concerns by patients and regulatory agencies about possible adverse psychiatric effects of 5-alpha-reductase inhibitor therapy. Discontinuation of these medications may be appropriate if depression develops.
Anticholinergic agents —
- alternative monotherapy for patients with predominately irritative symptoms (frequency, urgency, and incontinence) related to overactive bladder and without elevated postvoid residuals
- also used in combination therapy with alpha-adrenergic agents for patients with persistent symptoms of BPH who have irritative symptoms without elevated postvoid residuals.
- Tolterodine, oxybutynin, darifenacin, solifenacin, fesoterodine, and trospium are approved in the United States for overactive bladder.
- Alternatives include extended-release tolterodine, M3 selective drugs (eg, darifenacin, solifenacin), or quaternary amines (eg, trospium).
- side effects
- inhibition
of salivary secretion (dry mouth),
- blockade of the ciliary muscle of the lens to cholinergic stimulation (blurred vision for near objects),
- tachycardia,
- drowsiness,
- decreased cognitive function, and
- inhibition of gut motility and constipation.
- Anticholinergic agents are contraindicated in patients with gastric retention and angle-closure glaucoma.
Phosphodiesterase-5 inhibitors —
- reasonable to consider treatment with PDE-5 inhibitors in patients who have erectile dysfunction and mild or moderate symptoms (IPSS <20) of BPH.
- PDE-5 inhibitors can potentiate the hypotensive effects of alpha-1-adrenergic antagonists.
- improve lower urinary tract symptoms with inconsistent effects on urine flow rates compared
- A 2018 Cochrane review à PDE-5 inhibitors were not superior to alpha-blockers, and there was no benefit of adding PDE-5 inhibitors to therapy with either alpha-blockers or 5-alpha reductase inhibitors.
Combination Therapy
●For patients with severe symptoms of BPH (International Prostate Symptom Score [IPSS] ≥ 20)
who do not have an adequate response to maximal monotherapy with an alpha-adrenergic antagonist,
combination treatment with an alpha-adrenergic antagonist and 5-alpha-reductase inhibitor
●For men with low postvoid residual urine volumes and irritative symptoms (eg, frequency, urgency) that persist during treatment with an alpha-adrenergic antagonist, we suggest combination treatment with an anticholinergic agent.
●For men with moderate symptoms of BPH and erectile dysfunction, treatment with daily tadalafil (5 mg/day)alone or in combination with tamsulosin (0.4 mg/day)
Alpha-1-adrenergic antagonist and 5-alpha-reductase inhibitor —
- In patients with severe symptoms of BPH
- those who are known to have a large prostate (>40 mL), and/or
- in those who do not get an adequate response to maximal dose monotherapy with an alpha-adrenergic antagonist,
Alpha-1-adrenergic antagonist and anticholinergic —
For men with low postvoid residual urine volumes and irritative symptoms (e.g., frequency, urgency) that persist during monotherapy with an alpha-1-adrenergic antagonist or anticholinergic agent, we suggest combination treatment with an alpha-1-adrenergic antagonist and an anticholinergic agent.
Surgical Management
Patients who have persistent or progressive symptoms despite combination therapy for 12 to 24 months should be considered for surgical management. transurethral resection of the prostate (TURP)
