Myasthenia gravis
- autoimmune disorder affecting about I in 10,000 population
- development of antibodies directed to the nicotinic receptors (NR) at the muscle endplate.
- number of free NM cholino-receptors may be reduced to 1/3 of normal or less
- structural damage to the neuromuscular junction.
- Symptoms à weakness and easy fatigability on repeated activity, with recovery after rest.
- The eyelid, external ocular, facial and pharyngeal muscles are generally involved first.
- Later, limb and respiratory muscles get affected.
Diagnostic tests for myasthenia gravis
- Ameliorative test:
Initially, edrophonium 2 mg is injected i.v. as a test dose. If nothing untoward happens, the remaining 8 mg is injected after 30-60 sec.
Reversal of weakness and short-lasting improvement in the strength of affected muscles occurs only in myasthenia
gravis and not in other muscular dystrophies.
In case edrophonium is not available, the test can be performed with 1.5 mg i. v. neostigmine.
Atropine pretreatment may be given to block the muscarinic effects of neostigmine.
(b) Provocative test: myasthenics are highly sensitive to d-tubocurarine; 0.5 mg i.v. causes marked weakness
in them but is ineffective in non-myasthenics. This test is hazardous.
(e) Demonstration of anti- NR antibodies in plasma or muscle biopsy specimen is a more reliable test.
| Time to onset of effect* | Time to maximal effect* | |
| Symptomatic therapy | ||
| Pyridostigmine | 10 to 15 minutes | 2 hours |
| Chronic immunotherapies | ||
| Prednisone | 2 to 3 weeks | 5 to 6 months |
| Azathioprine | ~12 months | 1 to 2 years |
| Mycophenolate mofetil | 6 to 12 months | 1 to 2 years |
| Cyclosporine and tacrolimus | ~6 months | ~12 months |
| Rapid immunotherapies | ||
| Plasmapheresis | 1 to 7 days | 1 to 3 weeks |
| Intravenous immune globulin | 1 to 2 weeks | 1 to 3 weeks |
| Surgery | ||
| Thymectomy | 1 to 10 years | 1 to 10 years |
Overview of therapies — There are four primary therapies used to treat MG:
●Symptomatic treatment (acetylcholinesterase inhibition) to increase the amount of acetylcholine (ACh) available at the neuromuscular junction
●Chronic immunosuppressive therapies (glucocorticoids and nonsteroidal immunosuppressive agents) to target the underlying immune dysregulation
●Rapid but short-acting immunomodulating treatments (therapeutic plasma exchange and intravenous immune globulin [IVIG])
●Surgical treatment (thymectomy)
Treatment
1 . Acetylcholinesterase inhibition
- Neostigmine and its congeners are the first line drugs used to restore muscle strength.
- They improve muscle contraction by allowing ACh released from prejunctional endings to accumulate and act on the receptors over a larger area, as well as by directly depolarizing the endplate.
- Treatment is usually started with Neostigmine 15 mg orally 6 hourly; dose and frequency is then adjusted to obtain optimum relief from weakness.
- However, the dosage requirement may fluctuate from time to time and there are often unpredictable periods of remission and exacerbation.
- Pyridostigmine à less frequent dosing. (more preferred)
- The response to pyridostigmine is not uniform, however. In particular, most patients with muscle-specific tyrosine kinase (MuSK)-positive disease have a poor response to anticholinesterase agents.
- If intolerable muscarinic side effects are produced, atropine can be added to block them.
- These drugs have no effect on the basic disorder which often progresses; ultimately it may not be possible to restore muscle strength adequately with anti-ChEs alone.
- s/e – The most bothersome muscarinic side effects include abdominal cramping and diarrhea. Others are increased salivation and bronchial secretions, nausea, sweating, and bradycardia. Nicotinic side effects are also frequent and include fasciculations and muscle cramping
- Cholinergic crisis — A potential major side effect of excessive anticholinesterase medication is weakness, which can be difficult to distinguish from worsening MG.
If the dose of the antiChE is not adjusted according to the fluctuating requirement, relative overdose may
occur from time-to-time.
Overdose à weakness by causing persistent depolarization of muscle endplateà cholinergic weakness.
The two types of weakness require opposite treatments. They can be differentiated by edrophonium test
Inject edrophonium (2 mg. i.v.) à improvement à myasthenic crisis
- no improvement or worsening à cholinergic crisis
2. Immunosuppression
- Corticosteroid
improvement à immunosuppressant actionà inhibit production of antibodies to NR, and may increase synthesis of new NRs.
generally reserved for patients who do not respond adequately to anti-ChEs and have failed after thymectomy or are unsuitable for it.
Prednisolone 30–60 mg/day induces remission in about 80% of advanced cases. After tapering the dose, 10 mg daily or on alternate days can be used for maintenance therapy
- lmmunosuppressants à azathioprine and cyclosporine
Both inhibit NR-antibody synthesis by affecting T-cells.
Azathioprine is generally used first but has a slow onset of affect; may take months to induce a remission.
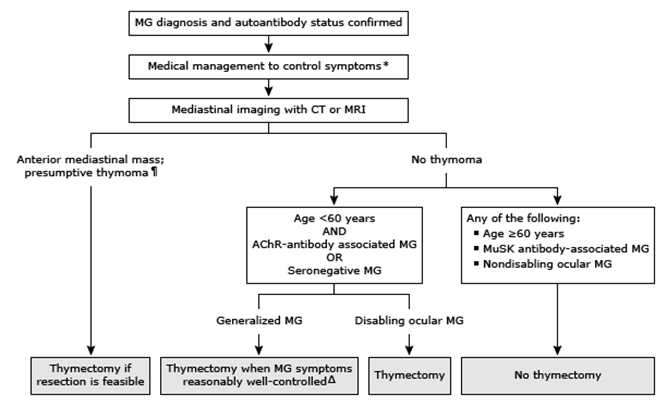
- Thymectomy
In the approximately 10 to 15 percent of patients with MG associated with a thymoma, surgery is indicated for patients in whom a complete resection is considered feasible.
generally advised for patients with generalised weakness, particularly for those with a thymoma and for younger patients.
- produces gradual improvement à and even complete remission has been obtained.
Thymus may contain modified muscle cells with Rs on their surface, which may be the source of the antigen for production of anti- R antibodies in myasthenic patients.
- plasmapheresis à Removal of antibodies by (plasma exchange) is another approach.
It may produce dramatic but often short-lived improvement
Myasthenic crisis is characterized by acute weakness of respiratory musclesà managed by tracheal intubation and mechanical ventilation.
Generally, i. v. methylprednisolone pulse therapy is given while anti-ChEs are withheld for 2- 3 days followed by their gradual reintroduction.
- Intravenous immune globulin (IVIG)
As with plasmapheresis, the effect of IVIG is seen typically in less than a week, and the benefit can last for three to six weeks.
IVIG is used in the same setting as plasmapheresis to quickly reverse a severe and life-threatening exacerbation of myasthenia.
total dose of IVIG is 2 g/kg, usually over two to five days.
Immunizations —
Patients with generalized MG who develop respiratory infections are at increased risk of myasthenic exacerbations and respiratory compromise
Current guidelines recommend annual seasonal influenza vaccination for all individuals receiving immunosuppressive therapy, and for those with neurologic conditions, including neuromuscular disorders such as generalized MG, or ocular MG within three years of onset, that can potentially compromise the handling of respiratory secretions.
The pneumococcal vaccine is recommended for all individuals with chronic pulmonary conditions and for those receiving immunosuppressive therapy.
| Drugs that may unmask or worsen myasthenia gravis |
| Anesthetic agents |
| Neuromuscular blocking agents¶ |
| Antibiotics |
| Aminoglycosides¶ (eg, gentamicin, neomycin, tobramycin) |
| Clindamycin |
| Fluoroquinolones (eg, ciprofloxacin, levofloxacin, norfloxacin) |
| Ketolides◊ (eg, telithromycin) |
| Vancomycin |
| Cardiovascular drugs |
| Beta blockers (eg, atenolol, labetalol, metoprolol, propranolol) |
| Procainamide |
| Quinidine |
| Other drugs |
| Anti-PD-1 monoclonal antibodies (eg, nivolumab and pembrolizumab) |
| Botulinum toxin |
| Chloroquine |
