Pharmacoeconomics
DEFINITION:
– “Analysis of the costs of drug therapy to health care systems and society.”
– “Assessing the implications of projected outcomes and costs of pharmaceutical products for the decision whether to continue or stop development of a drug and for global pricing strategy”
INTRODUCTION:
PE uses economic theories, concepts and tools and applies them in health and healthcare
- PE is not a cost saving tool
- PE allows rational resource allocation
- PE defines intervention with highest value
- PE helps to solve the clash between scare financial resources and growing healthcare demand
WHAT IS A PHARMACOECONOMIC EVALUATION OR HEALTH ECONOMIC EVALUATION?
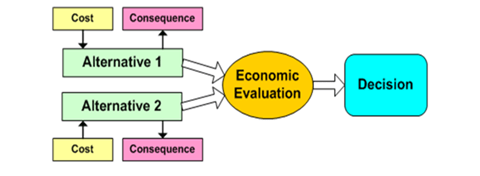
Refers to a study that considers both the comparative costs associated with two or more health care interventions, and the comparative clinical effects, measured either in clinical units, health preferences, or monetary benefit.
Challenges of healthcare financing health gap
Reasons for increasing healthcare costs:
- Demographic situation
- New technologies & innovation
- Increased levels of patient information
- Lifestyle (drug abuse, obesity, smoking)
- QoL expectations
- Higher affordability of healthcare
Why to study pharmacoeconomics?
- Expansion of medical knowledge
- Increase in treatment options
- Responsibility on the health care professionals to provide effective care efficiently
- Medical insurance or reimbursement systems
- Regulatory mandate
Pharmacoeconomic concept of value
Value = cost/outcomes
- Value is always seeked for a medical intervention, not only for a medication
- Value is always related to a specific disease and patient population.
Costs :
- Acquisition (drugs)
- Application
- Education
- Monitoring
- Patients costs
- Travel to hospital
- Absence at work
- Side effects
- Outpatient services
- Inpatient services
- Social allowances
- Productivity loss
- Remuneration loss
Outcomes :
- Clinical
- Reduction of events (Stroke, MI)
- Reduced mortality
- Improvement of score (HAQ)
- Quality of life
- Reduced disability
- Improvement of productivity
- Social integration
- Intangible outcomes
Costs:
Direct:
Medical
- Drugs
- Hospitalization
- Outpatient services
- Direct payments
- Lab, imaging.
Non-medical
- Transportation
- Accommodation
Indirect:
- Short term disability
- Productivity loss
- Long term disability
Intangible:
- Difficult to assess
- Pain
- Suffering
STAGES IN ECONOMIC EVALUATION:
Deciding upon study question
Assessment of costs and benefits
Adjustment of timing
Adjustment of uncertainty
Making a decision
TYPES OF ECONOMIC EVALUATIONS
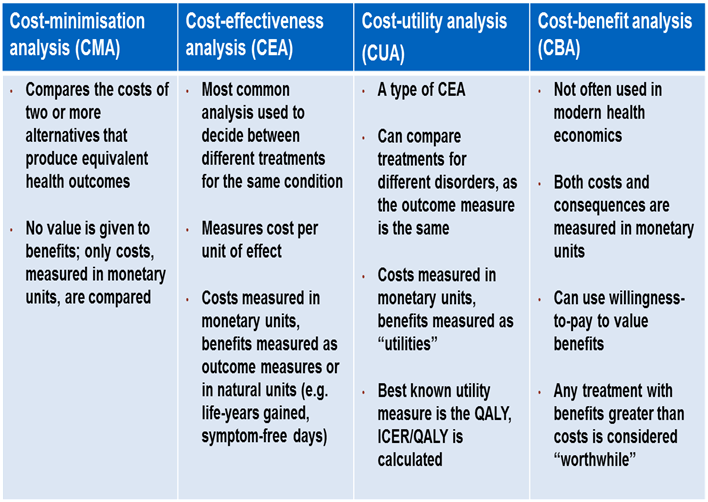
Cost-Minimization Analysis (CMA)
Cost-effectiveness Analysis (CEA)
Cost-Benefit Analysis (CBA)
Cost-Utility Analysis (CUA)
Cost Consequence Analysis (CCA)
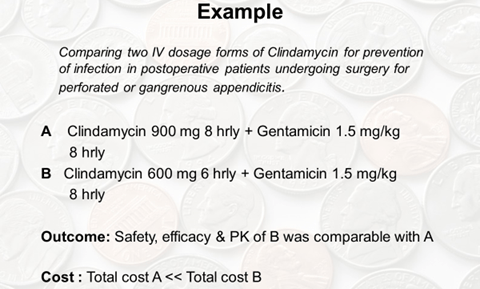
- Cost minimization analysis (CMA):
- Compares two (or more) interventions
- Searches the least costly technology (intervention) in terms of costs
- Necessity of same intervention outcome
- Least costly way to reach outcome
- Generic vs. original product
- Advantage:
- Simple
- Fast
- Disadvantage:
- Requires same outcomes therefore rarely applicable
- Cost effectiveness analysis (CEA):
- CEA consider both the costs and benefits of two treatment options.
- Measured in non-monetary terms.
- Expressed in natural units e.g., cost per years of life saved, cases cured.
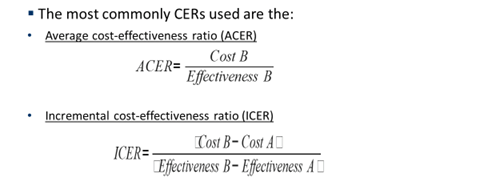
- Cost effectiveness ratio (CER) = Cost / Outcome
- Choice is that of treatment having lower CER
- Used to evaluate programs, therapies or services having common goals.
- However, CEA cannot compare between two different alternatives of treatment.
- Average cost-effectiveness ratio: Do not compare the costs and outcomes among health care alternatives.
- Incremental cost-effectiveness : Change in costs and health benefits when one health care intervention is compared to an alternative one Eg. Outpatient surgery vs. short-stay surgery
- ICER = Difference in the costs/ Difference in the effectiveness
Decision Making:
Two programs A (comparator) and B.
If Outcome B = Outcome A Compare costs (CMA)
If Outcome B > Outcome A and Cost B < Cost A, B is dominant
If Outcome B > Outcome A and Cost B > Cost A, we have to make a decision
In order to make a decision on which intervention to choose, a cost-effectiveness ratio (CER) should be calculated.
- Cost benefit analysis (CBA):
- To compare alternative therapies where outcome is different.
e.g., prolonging life and QoL
- Money – Common stable, consistent and plausible denominator
- Outcome = Benefit / Cost
- Most suitable when resources scarce and only one program can be implemented
- Measure of the benefit in CBA is expressed in monetary terms
- CBA not very common in pharmaco-economics
- Facilitate decision-making in that there is no need for a threshold
- All CB ratios < 1.0 are good and all CB ratios > 1.0 are bad.
- CBA are difficult to undertake
- Require willingness to pay methodology
- All outcomes cannot be converted into monetary terms
- CBA uses complex perspective and enables to compare intervention across disciplines
- CBA example:
Vaccine 1 à cost= 31,000 ; benefit= 35,000 so, CB Ratio =1.13
Vaccine 2 à cost= 25,000 ; benefit=24,000 so CB Ratio= 0.96
- COST UTILITY ANALYSIS (CUA):
- Utility is desirability for a particular state of health
- Basic purpose is to improve Quality of life in patients
- Accounts for physical, social and psychological well being
- Patient satisfaction
- Quality – Adjusted Life Year (QALY)
- Disability – Adjusted Life Year (DALY)
- When CUA…??
- if HRQoL is the relevant outcome
- comparable impact on morbidity and mortality (cancer)
- comparison across interventions
- limited budget
- maximation of QALY gain
- When CUA…??
EG Consider two treatments for Stage IV malignant melanoma
Treatment A:
- Survival 1 year
- Utility 0.7
- Costs 1.400
- Cost-utility for A:
- 1.400/(0.7 x 1) = 2.000 /QALY
Treatment B:
- Survival 1.2 year
- Utility 0.6
- Costs 2.160
- Cost-utility for B:
- 2.160/(0.6 x 1.2) = 3.000 /QALY
- Cost consequence analysis (CCA):
- An analysis in which resources and outcomes are calculated but not aggregated into cost outcome ratios
- Characteristics
- Resources are measured in monetary units
- Outcomes are measured in multiple ways
- Results are presented in a tabular format
- Advantages
- Transparency, Flexibility, Conceptually the simplest
Avoids controversies, Most comprehensive
- Limitations
- Labor/resource intensive
PE EVALUATIONS:
| Type | Advantages | Disadvantages |
| CMA | Simple | Same outcomes required |
| CEA | Option to use a variety of outcomes Can be compared to interventions with similar outcomes | Cannot be compared with interventions with different outcomes |
| CUA | Compares interventions with different outcomes – common denominator Patient´s perspective | Requires specific knowledge Difficult to use |
| CBA | Compares interventions with different outcomes | Difficult to state health status in monetary values |
To make it easy:
- It is cost minimization when I stand at the bar and choose the cheapest beer available.
- When I compare the price per liter to see which one satisfies my thirst for the least money this is a cost-effectiveness analysis.
- When I also take into account the flavor and alcoholic strength to decide which beer I prefer overall, I am performing a cost-utility study
- When I decide whether to buy a beer at all, to buy something else entirely, or save my money, and take into account the effect of the drink on my productivity the next day, that is a cost-benefit analysis
HOW PE IS APPLIED??
- Pharmaceutical industry
- Decision making during drug development
- Pricing a new medicine/ re-pricing an existing medicine
- Convincing the regulatory authorities for marketing approval
- Health policy makers
- Implied value and incremental cost-effective analysis are crucial while making health policy decisions.
- Economic analyses are used while programming budget
- Clinician & Common man
- Making an informed and rational choice of treatment