Pharmacotherapy of Sleep Disorders
- Sleep is a reversible behavioral state of perceptual disengagement from and unresponsiveness to the environment
- It constitutes a complex amalgam of physiologic and behavioral processes
It is typically accompanied by
- Postural recumbence
- Behavioral quiescence
- Eye closure
Problem statement
- 17 hours of sustained wakefulness blood alcohol level of 0.05%
- Associated with accidents and human errors
- 10–15% of fatal motor-vehicle crashes occur due to sleepiness or driver fatigue
- Night time use of TV, mobile phones à Sleep problems
- Cognitive impairment seen with sleep disorders
- Associated with short and long-term effects on health and well-being and quality of life
- Sleep à NREM and REM type à Sleep cycle
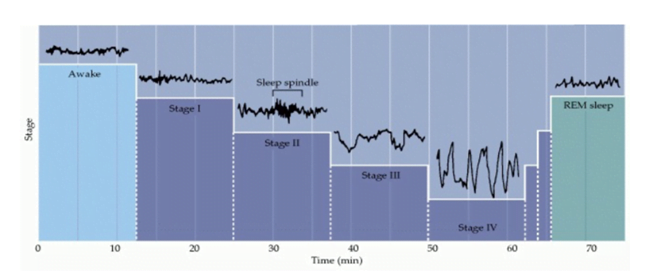
- waking state à eyes open à high-frequency (15–60 Hz), low-amplitude activity (~30 μV) activity à beta activity
- Descent into stage I non- REM sleep à decreasing EEG frequency (4–8 Hz) and increasing amplitude (50–100 μV) à theta waves
- Descent into stage II non-REM sleep à by 10–15 Hz oscillations (50–150 μV) called spindles, which occur periodically and last for a few seconds
- Stage III non-REM sleep à slower waves at 2–4 Hz (100–150 μV)
- Stage IV sleep is defined by slow waves à delta waves at 0.5–2 Hz (100– 200 μV)
- REM sleep à low-voltage, high-frequency activity similar to the EEG activity of individuals who are awake
- Each sleep cycle lasts for about 90 mins. Max time about 40-50% spent in phase II. REM sleep 20-25 %, Most prominent phase is the slow wave sleep (Stage IV). Duration of REM sleep increases as one grows up.
- five neurotransmitters : histamine, dopamine, norepinephrine, serotonin, and acetylcholine à ascending reticular activating system, because they are known to work together to regulate arousal
Insomnia
- defined in ICSD-3 as a complaint of trouble initiating or maintaining sleep which is associated with day-time consequences and is not attributable to environmental circumstances or inadequate opportunity to sleep
- The disorder is identified as chronic when it has persisted for at least three months at a frequency of at least three times per week.
- DSM-V: 3 nights/week; 1 months but < 3 months: episodic, >3 months persistent insomnia
- Insomnia is a more prevalent à females than among males, with a gender ratio of about 1.44:1.
- Insomnia is a common comorbidity of many medical conditions, including diabetes, coronary heart disease, chronic obstructive pulmonary disease, arthritis, fibromyalgia, and other chronic pain conditions. The risk relationship appears to be bidirectional: insomnia increases the risk of medical conditions, and medical problems increase the risk of insomnia.
- Diagnosis à Polysomnography usually shows impairments of sleep continuity Eg: increased sleep latency, decreased stages 3 and 4 sleep
General treatment measures
- Treatment of comorbid medical and psychiatric conditions
- Modifying sleep interfering medications
- Optimizing the sleep environment
Specific treatment of insomnia
- Cognitive Behavioral Therapy (CBT)
- Pharmacotherapy
- Indian psychiatry guidelines: For the short-term insomnia, pharmacotherapy is indicated, while for the chronic insomnia, cognitive behavior therapy for insomnia (CBT-I) is preferred.
CBT-I
- Education regrading sleep physiology and sleep hygiene
- Addressing dysfunctional beliefs
- Stimulus control therapy
- Sleep restriction
- Relaxation training
- Maintaining sleep diary to monitor therapy
Pharmacotherapy of insomnia
First line therapy
- Short/intermediate acting benzodiazepines or newer BZD receptor agonistic modulators [BzRAs] or Ramelteon
Second line therapy
- Other drugs, such as sedating antidepressants or anticonvulsant medications particularly when comorbidities (e.g. mood disorder or epilepsy) are present
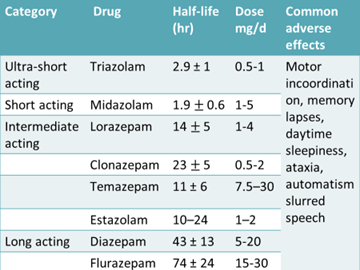
Benzodiazepines
- The lack of direct channel activation by benzodiazepines and their dependence on the presynaptic release of GABA at the GABAA receptor likely contribute to the safety of these agents as compared to barbiturates.
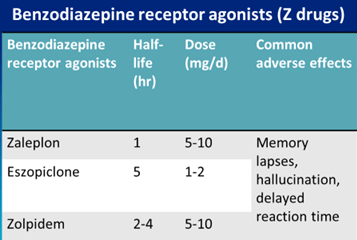
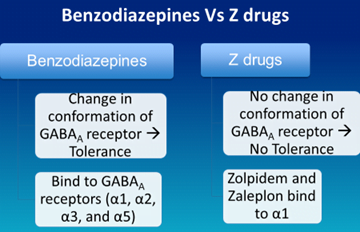
- Z drugs do not disturb the sleep architecture
- Despite the shortening of durations of stage 4 and REM sleep, benzodiazepine administration typically increases total sleep time, largely by increasing the time spent in stage 2, which is the major fraction of non-REM sleep. Decrease REM sleep time but increase the number of cycles
- Chronic benzodiazepine use poses a risk for development of dependence and abuse
- Tolerance has been observed with all currently licensed hypnotics with the exception of melatonin
- If used for more than 3 weeks, withdraw slowly
- Overdose: Flumazenil
Melatonergic drugs
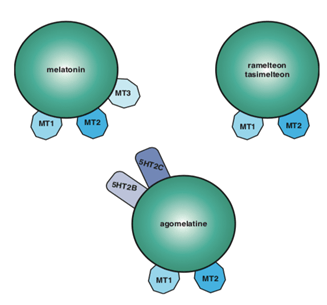
- Endogenous melatonin à secreted by the pineal gland
- mainly acts in the suprachiasmatic nucleus to regulate circadian rhythms.
- three types à melatonin 1 and 2 (MT1 and MT2), which are both involved in sleep, and
- melatonin 3 à not thought to be involved in sleep physiology.
- Ramelteon is efficacious in combating both transient and chronic insomnia, with no tolerance occurring in its reduction of sleep onset latency even after 6 months of drug administration
- Agomelatine withdrawn from due to US due to hepatic impairment
- Agomelatine is not only an MT1 and MT2 receptor agonist, but is also a 5HT2C and 5HT2B receptor antagonist and is available as an antidepressant in Europe
Tricyclic antidepressants
- Doxepin
- at antidepressant doses (150–300 mg/day), inhibits serotonin and norepinephrine reuptake and is an antagonist at histamine 1, muscarinic 1, and α1-adrenergic receptors.
- At low doses (1–6 mg/day), however, doxepin is quite selective for histamine 1 receptors and thus may be used as a hypnotic.
- taken in initial doses of 6 mg (3 mg in the elderly) within 30 min of bedtime
- Approved by the FDA in 2010 for the treatment of sleep maintenance insomnia.
- ADRs: Abnormal thinking and behavior have been observed following its use, and it can worsen suicidal ideation and depression.
Orexin antagonists à Suvorexant
- neurotransmitter orexin (also called hypocretin) is made by cells located in the hypothalamus
- Approved by US FDA in 2014
- Not available in india
- s/e à Daytime somnolence, Possibility of the worsening of depression or suicidal ideation
Off label drugs
- Chlorpromazine, Diphenhydramine, Promethazine
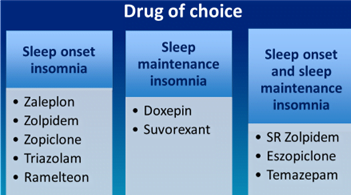
- In general, short acting à sleep onset
- However, intermediate and long acting agents à residual daytime effects and may produce the somnolence during the day
- Data is available for treatment with Z drugs for as long as 6 months without any major adverse effects. Considering the limited availability of trained CBT-I therapist, consensus was reached that in certain circumstances where CBT-I is not possible for any reason, pharmacothepray may be instituted for long term
- For short term insomnia, patient should be requested to give drug holidays intermittently and to restart the treatment when the symptoms appear again. CBT stopped when patient stabilized for atleast 4 weeks
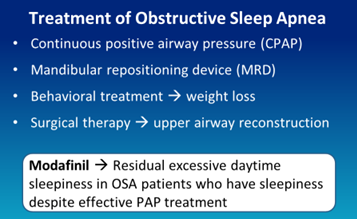
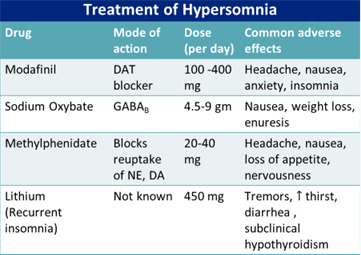
Modafinil à block dopamine transporter (DAT)
- increase in synaptic dopamine following blockade of DAT leads to increased tonic firing and downstream effects on neurotransmitters including those involved in wakefulness, such as histamine and orexin/hypocretin.
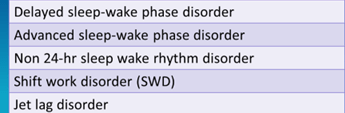
Circadian rhythm sleep-wake disorders (CRSD)
- Melatonin agonist à Tasimelteon
Parasomnias
- sleep disorders defined as undesirable physical events or experiences that occur during the initiation of sleep, during sleep or during arousal from sleep
- REM related parasomnias – Nightmare disorder, REM sleep behavior disorder (RBD)
- NREM related parasomnias – Sleep walking, sleep terrors, sleep related eating disorder
- Other à sleep enuresis
- The only REM-sleep parasomnia where pharmacotherapy is clearly indicated is RBD
- Drug of choice for RBD: Clonazepam and Melatonin; Mechanism of action of melatonin in RBD is not known à calmodulin antagonism?
Sleep enuresis
- Bed wetting alarm
- Positive reinforcement
- Desmopressin: 0.2 mg tablet/ 20 mcg nasal sprays
- Imipramine: 50-75 mg
