Hypertension
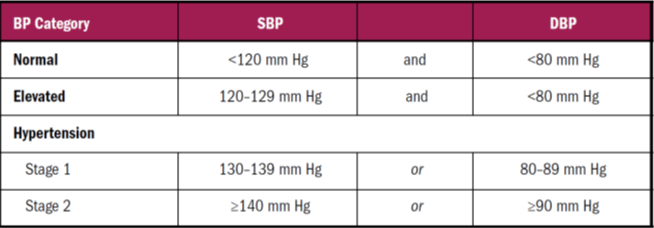
Almost all HT management guidelines including NICE (20 11 ). JNC8 (20 14), WHO-ISH (2003). European Society of Hypertension (2007, 2013) define the cut-off level to be 140 mm Hg systolic and 90 mm Hg diastolic.
However, the JNC8 have raised the defining level to 150/90 mm Hg for individuals above 60 years of age.
- Blood pressure is the product of cardiac output and total peripheral resistance (TPR).
- Cardiac output is dependent on total blood volume, heart rate and the pumping action of the heart whereas peripheral resistance is determined by the diameter of arterioles (vasoconstriction leads to increase in TPR).
- Sympathetic system stimulates the heart directly (β1), causes vasoconstriction (α) and also stimulates the renin-angiotensin aldosterone system (β1 stimulates renin release).
- All these factors result in increased blood pressure.
- Four main group of drugs used for controlling hypertension are,
- diuretics (decrease blood volume and sodium retention),
- sympathoplegics,
- vasodilators and
- the agents decreasing the activity of renin-angiotensin aldosterone system (RAAS).
Classification
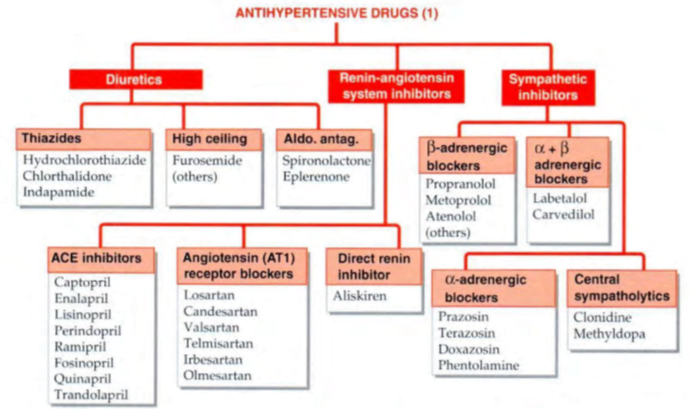
DIURETICS
- Thiazides (hydrochlorothiazide, chlorthalidone) à diuretic of choice for uncomplicated hypertension; have similar efficacy and are dose to dose equivalent.
- All megatrials have been carried out with these two only.
- Chlorthalidone is longer acting (~ 48 hours) than Hydrochlorothiazide (< 24 hours) and may have better round-the-clock action.
- Indapamide à equally effective.
mechanism of antihypertensive action is:
1. Initially, the diuresis reduces plasma and e.c.f. volume by 5–15%, and this decreases c.o.
2. Subsequently, compensatory mechanisms operate to almost regain Na+ balance and plasma volume; c.o. is restored, but the fall in BP is maintained by a slowly developing reduction in t.p.r.
3. Decrease in intracellular Na+ concentration in the vascular smooth muscle may reduce stiffness of vessel wall, increase their compliance and dampen responsiveness to constrictor stimuli (NA, Ang II).
- Similar effects are produced by salt restriction; antihypertensive action of diuretics is lost when salt intake is high.
- fall in BP develops gradually over 2–4 weeks.
- Thiazides are mild antihypertensives, average fall in mean arterial pressure is ~10 mm Hg.
- They are effective by themselves in ~ 30% cases (mostly low grade hypertension) but they potentiate all other antihypertensives (except DHPs) and prevent development of tolerance to these drugs by not allowing expansion of plasma volume.
- Thus, in combination, they are useful in any grade of hypertension.
High ceiling diuretics à Furosemide
- strong diuretic, but the antihypertensive efficacy does not parallel diuretic potency.
- weaker antihypertensive than thiazides: fall in BP is entirely dependent on reduction in plasma volume and c.o.
- The explanation to this paradox may lie in its brief duration of action.
- The natriuretic action lasting only 4–6 hr after the conventional morning dose is followed by compensatory increase in proximal tubular reabsorption of Na+.
- The Na+ deficient state in vascular smooth muscle may not be maintained round-the-clock. The t.p.r. and vascular responsiveness are not reduced.
- high ceiling diuretics are more liable to cause fluid and electrolyte imbalance, weakness and other side effects.
- indicated in
- hypertension only when it is complicated by:
- (a) Chronic renal failure: thiazides are ineffective, both as diuretic and as antihypertensive.
- (b) Coexisting refractory CHF.
- (c) Resistance to combination regimens containing a thiazide
Desirable properties of thiazide diuretics as antihypertensives are:
1. Once a day dosing and flat dose-response curve permitting simple standardized regimens.
2. No fluid retention, no tolerance.
3. Low incidence of postural hypotension
4. Effective in isolated systolic hypertension (ISH).
5. Lessened risk of hip fracture in the elderly due to hypocalciuric action of thiazides.
6. Low cost.
usual dose used was hydrochlorothiazide/ chlorthalidone 50 mg/day.
Side effects
• Hypokalaemia—muscle pain, fatigue and loss of energy.
• Erectile dysfunction in males.
• Carbohydrate intolerance: due to inhibition of insulin release (probably secondary to K+ depletion which interferes with conversion of proinsulin to insulin), precipitation of diabetes.
• Dyslipidemia: rise in total and LDL cholesterol and triglycerides with lowering of HDL. This
could increase atherogenic risk, but no direct evidence has been obtained.
• Hyperuricaemia: by inhibiting urate excretion— increased incidence of gout.
Over the past 25 years thiazides have been used at lower doses (12.5–25 mg/day hydrochlorothiazide or equivalent) alone and in combination with a K+sparing diuretic.
- All side effects mentioned above – low incidence with low dose
JNC 8
- low-dose (12.5–25 mg) thiazide therapy, preferably with added K+ sparing diuretic, as a first choice treatment of essential hypertension, especially in the elderly.
- Higher doses are neither more effective nor safe.
- If the low dose (25 mg/day) fails to reduce BP to desired level, another antihypertensive should be added, rather than increasing dose of the diuretic.
- Thiazides are ineffective in patients with chronic kidney disease (C KD), and are not recommended.
- High-ceiling diuretics are effective in patients with Clcr 30 mg/ml or less, and may be used in place of HCZ.
Potassium sparing diuretics
- Spironolactone, eplerenone and amiloride but not triamterene themselves lower BP slightly.
- However, they are used only in conjunction with a thiazide diuretic to prevent K+ loss and to augment the antihypertensive action.
- Spironolactone is not favoured because of its hormonal side effects (gynaecomastia, impotence, menstrual irregularities).
- Hyperkalemia should be watched when K+ sparing diuretics are used with ACE inhibitors/ARBs.
The NICE and JNC 8 guidelines recommend adding an aldosterone antagonist to the ACE inhibitor/ARB + CCB + thiazide regimen, if the target level BP is not attained
ANGIOTENSIN CONVERTING ENZYME (ACE) INHIBITORS
- one of the first-choice drugs in all grades of essential as well as renovascular hypertension
- Used alone they control hypertension in ~50% patients, and addition of a diuretic/β blocker extends efficacy to ~90%.
- Because of supra-additive synergism, only a low dose of diuretic (12.5 mg of hydrochlorothiazide, rarely 25 mg) needs to be added.
- renal blood flow improving action, their potential to retard diabetic nephropathy and their capacity to regress left ventricular/vascular hypertrophy.
- most appropriate antihypertensives in patients with
- diabetes, nephropathy (even nondiabetic), left ventricular hypertrophy, CHF, angina and post MI cases
- They appear to be more effective in younger (< 55 year) hypertensives than in the elderly, as well as in while races than in blacks.
ANGIOTENSIN RECEPTOR BLOCKERS
- In a dose of 50 mg/day losartan is an effective antihypertensive.
- Action manifests early and progresses to peak at 2–4 weeks.
- Addition of 12.5 mg/day hydrochlorothiazide further enhances the fall in BP.
- The newer ARBs—valsartan, candesartan, irbesartan and telmisartan have been shown to be as effective antihypertensives as ACE inhibitors, while losartan may be somewhat weaker than high doses of ACE inhibitors.
- Because they do not increase kinin levels, the ACE inhibitor related cough is not encountered.
- Angioedema, urticaria and taste disturbance are also rare.
- As antihypertensive, use of ARBs has outstripped that of ACE inhibitors.
- The NICE (201 1) guidelines consider ARBs to be preferable over ACE inhibitors for black races.
- Both JNC8 and NICE recommend not to combine ACE inhibitors with ARBs for hypertension.
DIRECT RENIN INHIBITORS à Aliskiren
- RAS inhibitors which act by blocking catalytic activity of renin and inhibiting production of Ang I and Ang II
- no remarkable features have emerged
- employed when the more established ACE inhibitors or ARBs cannot be used, or to supplement them.
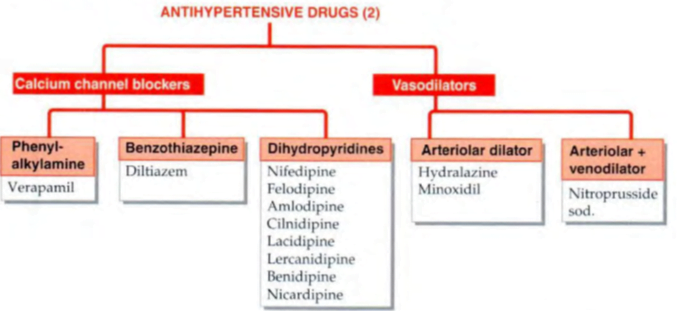
CALCIUM CHANNEL BLOCKERS
- All 3 subgroups of CCBs, viz. dihydropyridines (DHPs, e.g. amlodipine), phenylalkylamine (verapamil) and benzothiazepine (diltiazem) are equally efficacious antihypertensives.
- They lower BP by decreasing peripheral resistance without compromising c.o.
- Despite vasodilatation, fluid retention is insignificant.
- Monotherapy with CCBs is effective in ~ 50% hypertensives;
Advantages of CCB:
- 1. Do not compromise haemodynamics: no impairment of physical work capacity.
- 2. No sedation or other CNS effects; cerebral perfusion is maintained.
- 3. Not contraindicated in asthma, angina (especially variant) and PVD patients
- 4. Do not impair renal perfusion.
- 5. Do not affect male sexual function.
- 6. No deleterious effect on plasma lipid profile, uric acid level and electrolyte balance.
- 7. Shown to have no/minimal effect on quality of life.
- 8. No adverse foetal effects; can be used during pregnancy (but can weaken uterine contractions during labour).
- first line monotherapy options (JNC8, 2014) because of their high efficacy and excellent tolerability.
- most useful antihypertensives in cyclosporine induced hypertension in renal transplant recipients.
- However, the negative inotropic and dromotropic action of verapamil and diltiazem may worsen CHF and cardiac conduction defects, but DHPs are safe
β-ADRENERGIC BLOCKERS
- mild antihypertensives; do not significantly lower BP in normotensives.
- Used alone they suffice in 30–40% patients—mostly stage I cases.
- hypotensive response to β blockers develops over 1–3 weeks
- All β blockers, irrespective of associated properties, exert similar antihypertensive effect.
- Drugs with intrinsic sympathomimetic activity (ISA) cause less/no reduction of HR and c.o. but lower vascular resistance by β2 agonism.
- Nebivolol reduces t.p.r. by generating NO.
- The nonselective β blockers slightly reduce renal blood flow and g.f.r., but this is minimal in the β1 selective blockers and in those with ISA
- Nonselective ß blockers have an unfavourable effect on lipid profile (raise triglyceride level and LDL/HDL ratio).
- also fared less well on quality of life parameters like decreased work capacity, fatigue, loss of libido and subtle cognitive effects (forgetfulness. low drive), nightmares and increased incidence of antidepressant use.
- As monotherapy, ACE inhibitors/ARBs and CCBs appear to compromise quality of life less than B blockers.
- Rebound hypertension has occurred on sudden discontinuation of B blockers; myocardial ischaemia may be aggravated and angina or MI may be precipitated.
- B blockers are no longer considered first line antihypertensive drugs for monotherapy (JNC 8)
β+α ADRENERGIC BLOCKERS
Labetalol
- combined α and β blocker
- reduces t.p.r. and acts faster than pure β blockers.
- used i.v. for rapid BP reduction in hyperadrenergic states, cheese reaction, clonidine withdrawal, eclampsia, etc.
- Oral labetalol therapy is restricted to moderately severe hypertension not responding to a pure β blocker, because side effects of both α blocker and β blocker occur with it.
Carvedilol à has additional antioxidant/free radical scavenging properties.
α-ADRENERGIC BLOCKERS
Prazosin
- Dilates both resistance and capacitance vessels; effect on the former predominating.
- The haemodynamic effects, viz reduction in t.p.r. and mean BP accompanied by minor decrease in venous return and c.o. are similar to that produced by a direct acting vasodilator
- postural hypotension and fainting may occur in the beginning—called ‘first dose effect’, and with dose increments.
- This disappears with continued therapy, but may persist in the elderly.
- For this reason, prazosin is always started at low dose (0.5 mg) given at bedtime and gradually increased with twice daily administration till an adequate response is produced (max. dose 10 mg BD).
- advantages of prazosin are:
• Does not impair carbohydrate metabolism; suitable for diabetics, but not if neuropathy is present, because postural hypotension is accentuated.
• Has a small but favourable effect on lipid profile: lowers LDL cholesterol and triglycerides, increases HDL.
• Affords symptomatic improvement in coexisting benign prostatic hypertrophy.
Adverse effects
- postural hypotension
- headache, drowsiness, dry mouth, weakness, palpitation, nasal blockade, blurred vision and rash.
- Ejaculation may be impaired in males: especially
Use Prazosin is a moderately potent antihypertensive, but is not used as a first line drug because fluid retention and tolerance gradually develops
Nonselective alpha blockers (Phentolamine, Phenoxybenzamine)
- reserved for special situations like pheochromocytoma, clonidine withdrawal, cheese reaction, etc., where circulating CAs are responsible for the rise in BP.
DRUGS INHIBITING CENTRAL SYMPATHETIC OUTFLOW
- Stimulation of α2 receptors in CNS leads to decrease in sympathetic outflow whereas stimulation of β receptors in the brain has opposite effects.
- Therefore, α2 agonists and β1 antagonists can decrease the sympathetic activity and are useful for the treatment of hypertension.
- Clonidine and α-methyl dopa act as α2 agonists in the brain.
- Clonidine acts directly whereas the effect of α methyl dopa is due to its conversion to α methyl norepinephrine (α methyl dopa is a prodrug and converted to its active metabolite in the brain).
- Both of these drugs can cause sedation.
- Abrupt discontinuation of clonidine therapy can lead to rebound hypertension (treated by phentolamine); therefore this drug is not suitable for people having travelling job like business executives who are likely to miss the doses.
- Both of these drugs are safe in pregnancy (α methyl dopa is preferred).
- New drugs like moxonidine and rilmenidine are congeners of clonidine with longer half lives.
Other indications
1. Opioid withdrawal: Opioid and α2 adrenergic systems converge on the same effectors in many systems; both activate the Gi regulatory protein. Clonidine suppresses sympathetic overactivity of opioid withdrawal syndrome and reduces craving to some extent.
Clonidine has also facilitated alcohol withdrawal and smoking cessation.
2. Clonidine has analgesic activity à substitute morphine for intrathecal/epidural surgical and postoperative analgesia.
3. Clonidine attenuates vasomotor symptoms of menopausal syndrome.
4. control loose motions due to diabetic neuropathy.
VASODILATORS à
Drugs may cause vasodilation by
- opening potassium channels,
- by releasing nitric oxide,
- by blocking calcium channels or
- by acting as agonists of dopamine receptors.
- These drugs may be mainly arteriolar dilators (hydralazine, minoxidil, calcium channel blockers, diazoxide, fenoldopam), mainly venodilators (nitrates) or may dilate both arterioles and venules (sodium nitroprusside, ACE inhibitors, ARBs, α-blockers).
- All vasodilators can lead to reflex tachycardia due to vasodilation and sodium and fluid retention due to compensatory mechanisms; therefore these are best utilized in combination with diuretics and beta blockers.
A. POTASSIUM CHANNEL OPENERS
- hydralazine, minoxidil and diazoxide.
- By opening potassium channels, these drugs cause dilatation of mainly arterioles. These have negligible effect on venules.
- Hydralazine in addition acts by releasing nitric oxide (NO) from the endothelium.
- Minoxidil and hydralazine can be given orally for the treatment of severe hypertension whereas diazoxide is administered in hypertensive emergencies as rapid i.v. injection.
- Hydralazine is metabolized by acetylation and thus its effect is genetically determined due to the presence of slow and fast acetylators.
- On prolonged administration it can lead to drug induced lupus erythematosis.
- Minoxidil is a prodrug and is activated in liver to produce minoxidil sulphate (by phase II reaction), which opens potassium channels. Its levels are not changed in renal disease, so it is particularly useful in patients with chronic renal failure.
- Minoxidil can cause abnormal hair growth in females (hirsutism) and this adverse effect has been utilized as a treatment of alopecia in males.
- Diazoxide is a thiazide derivative and can cause hyperuricemia and hyperglycemia (by inhibiting insulin release from beta cells of pancreas). The latter effect has lead to its use in insulinoma.
B. NO RELEASERS
- Sodium nitroprusside and hydralazine act by releasing nitric oxide from the endothelium,
- increases intracellular cGMP by stimulation of guanylyl cyclase leading to vasodilation.
- Nitroprusside, in addition can directly stimulate guanylyl cyclase to cause increase in cGMP.
- Nitroprusside is a very short acting drug; therefore has to be administered by constant i.v. infusion for the treatment of hypertensive emergencies.
- Its solution should be freshly prepared because it is unstable and sensitive to light.
- Prolonged administration of this drug can result in accumulation of cyanide leading to toxicity particularly in patients with renal disease.
- It can also result in hypothyroidism due to the accumulation of thiocyanate (antithyroid compound). It is contra-indicated in pregnancy.
C. DOPAMINE AGONIST
- Fenoldopam is dopamine D1 receptor agonist that causes dilation of peripheral arteries and natriuresis.
- can be used i.v. for short term control of blood pressure in hypertensive emergencies particularly in patients with renal dysfunction (because of improved renal perfusion).
- It can increase intraocular pressure and hypokalemia has also been reported with the use of this drug.
American College of Cardiology/American Heart Association 2017