Evaluation of diuretics
- Diuresis: Increased excretion of urine. Natriuresis: Increased excretion of Sodium. Saluresis: increased excretion of Na and Cl.
Indications of Diuretics
- Hypertension (Thiazides)
- Chronic heart failure, cirrhosis, nephrotic syndrome (Loop diuretics)
- Acute pulmonary oedema (Loop diuretics)
- Nephrogenic diabetes insipidus (Thiazides)
- I & II hyperaldosteronism (K sparing)
- Need for newer diuretics is linked to drawbacks of current diuretics
- Hypovolemia, electrolyte imbalance, metabolic changes, impotence, hyperuricemia, drug allergy
- Diuretic resistance: increased absorption distally if NaCl absorption is inhibited proximally. When the luminal conc of diuretic is decreased the nephron compensates by increasing Na resorption. Ability to induce dieresis declines overtime since there is concomitant depletion of extracellular fluid and structural & functional changes in the nephron.
Ideal Diuretics
Aim of evaluating a diuretic
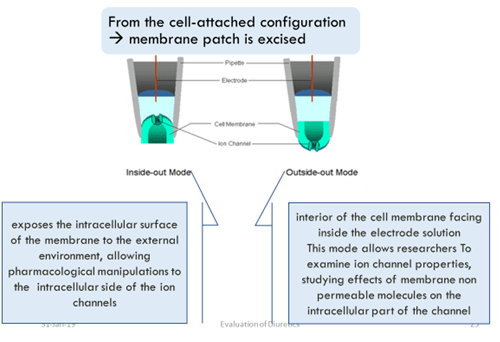
- Net flux of various ion across tubular epithelium
- Transcellular electrical gradient
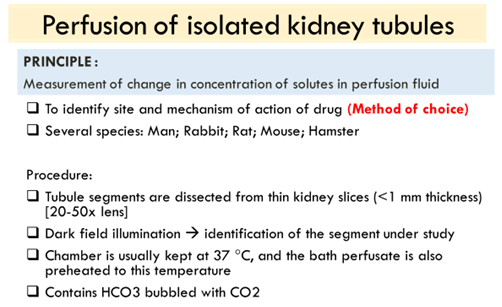
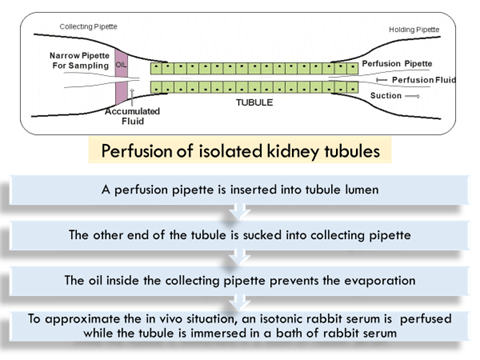
- Rat or dog kidney
- Evaluating activity in PCT
- Kidneys dissected and perfused using dialysing unit
- Perfusion pressure of 80-90 mm Hg and ureters are cannulated
- Renal artery is cannulated via the superior mesenteric artery
- Clearance periods of 20 min à urine samples
- Perfusates are collected at midpoints
- Electrolytes are measured by flame photometry
- Fractional excretions of water, electrolytes and test compounds are calculated
- Nishiitsutsuji-Uwo et al. (1967) – Metabolic activities of the isolated perfused rat kidney were described
- Cox et al. (1990) – the isolated perfused rat kidney as a tool in the investigation of renal handling and effects of nonsteroidal anti-inflammatory drugs
IN VIVO
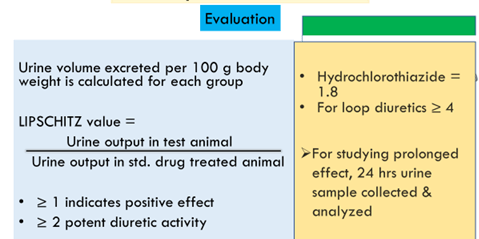
- Diuretic activity in rats (Lipschitz method):
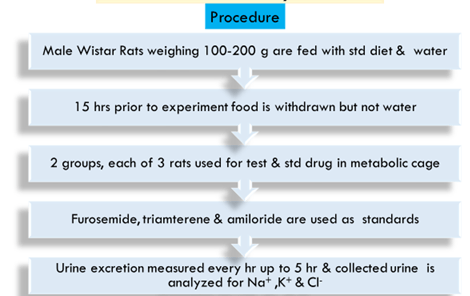
- Diuretic activity in Rats (Male Wistar of 100-200 g)
- Principle: Based on water and sodium excretion in test animals and compared to rats treated with a high dose of urea
Procedure:
- Rats are fed with standard diet & water
- 15 hr. before the experiment, food & water are withdrawn
3 animals per group in metabolic cages
- Metabolic cages :
- Wire mesh at bottom
- Funnel to collect urine
- Stainless-still sieves placed into the funnel to retain feces and to allow the urine to pass
Parameters :
- Urine excretion recorded up to 5 hr & 24 hr.
- Na+ content of urine estimated by flame photometer & Urine vol. excreted calculated for each group
Modification
- Cummings et al (1960) à sequential procedure with criteria for acceptance or rejection of test drugs
- Klatt et al (1975) à collection of urine excreted by cats
- Kau et al (1984) à screening diuretic agents in the rat using normal saline (4% body weight) as hydrating fluid
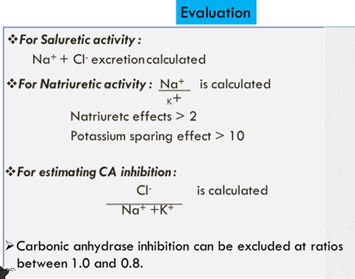
Saluretic activity in rats:
- Excretion of electrolytes is important for the treatment of peripheral edema, CHF, hypertension
- diuretic with saluretic & K+ sparing effects are needed
- Diuresis test in rats is designed to determine Na+ ,K+ , Cl– , water content & osmolarity of urine
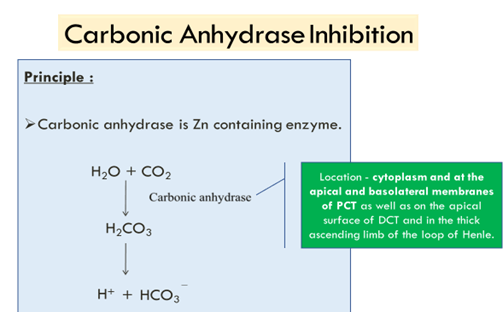
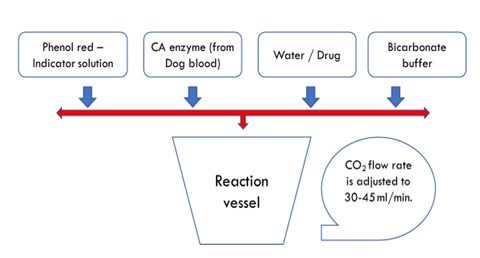
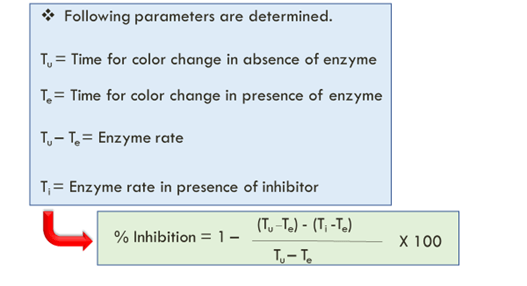
- Ratio b/w electrolytes can be calculated indicating carbonic anhydrase inhibition or K+ sparing effect
- Confirmatory methods:
- Diuretic and saluretic activity in dogs: Beagle dogs are used and need excessive training for accepting gavage feeding and urine collection with catheterization without resistance. Placed in metabolic cages. Stop food and water 24 hrs before exp. Drinking water is given in 20 mL/kg loading f/b 4 mL/kg hourly. ½ hourly urine samples are collected in the 1st hour to record baseline values. Test/control given. 1 hourly sample is collected till 6hrs. Then animals placed in metabolic cages and urine collected 24 hrs later.
- Na and K (flame photometry), Cl (chloride titrator) and osmolality (osmometer) are measured
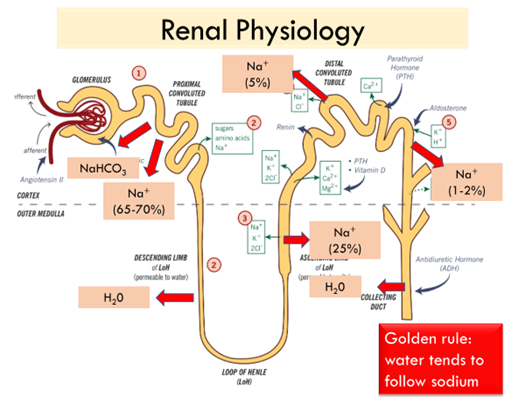
- In-vivo studies for determining MOA:
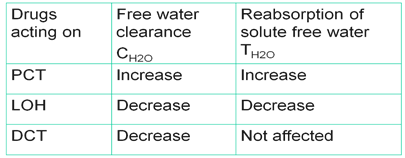
- Clearance method: Beagle dogs are used. Two conditions are created in the dogs namely water dieresis (by water loading) and water restriction (by water restriction for 48 hr) and clearance of solute free water and re-absorption of solute free water is determined.
Evaluation
- Water and electrolyte excretion
- Glomerular filtration rate : Inulin is used
- Renal plasma flow : Para amino hyppurate is used
- CH20 & TCH2O
- Clinical evaluation:
- Subjects:
- Phase 1: Healthy volunteers/Patients hospitalized for non-renal diseases
- Phase 2 and 3: edematous patients
- It is crucial to achieve a steady state of water and electrolyte metabolism: hence a standardized diet is given which supplies 70-80 mEq/d Nacl and 1.5 -2 L fluid intake/d for 72 hrs prior to the study. Daily monitoring of urine electrolytes is done so that 90% of Na is excreted.
- Parameters –
- Body weight (Baseline, at the time of final trial drug administration)
- Pharmacological Outcome Variables –
- Urine volume
- Urine osmolality
- Quantitative examination of urine
- Biochemical examination of blood
- Design:
- Single dose: For onset and duration of action
- Ascending dose: gives DR relationship, tolerability and MTD
- PK factors: Determination of plasma and urinary conc of the drug and metabolite which gives us an idea about the absorption and excretion. Also effect of pathological conditions like RF or nephritic syndrome should be studied.
- Parameters:
- Urine volume, Urine electrolytes and free water clearance: Give an idea of the MOA
- Weight loss, effect on GFR and RPF
- ADR profile
Outcome measures:
- Change in Serum Creatinine from baseline
- Change in Weight
- Proportion of Patients Free of Congestion
- Patient Well Being, as determined by a Global VAS
- Change in Cystatin C
- Change in Uric Acid
- Change in B-type Natriuretic Peptide
- Net Fluid Loss
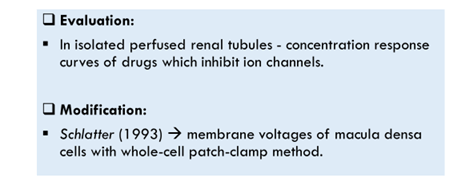
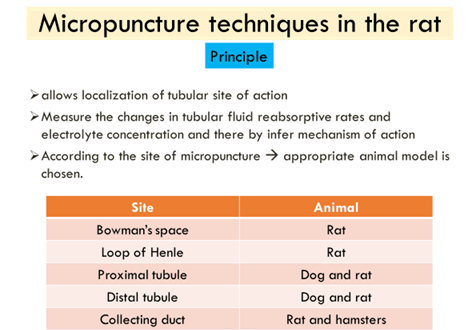
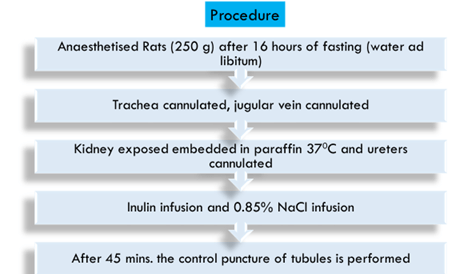
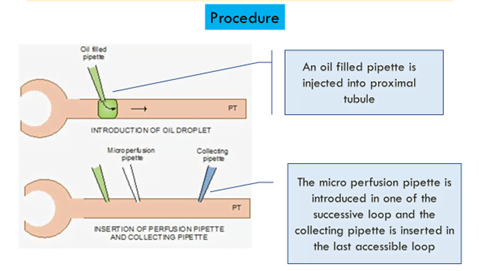
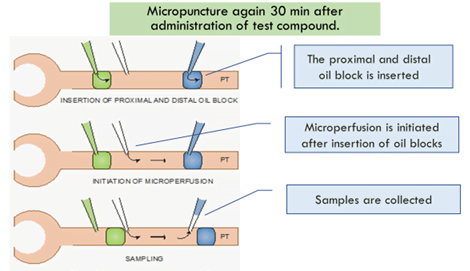
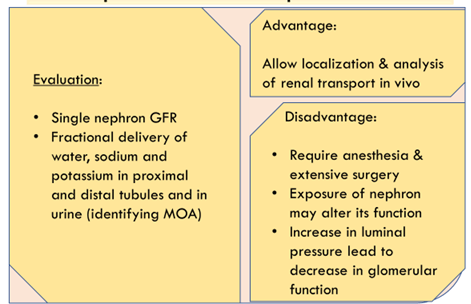
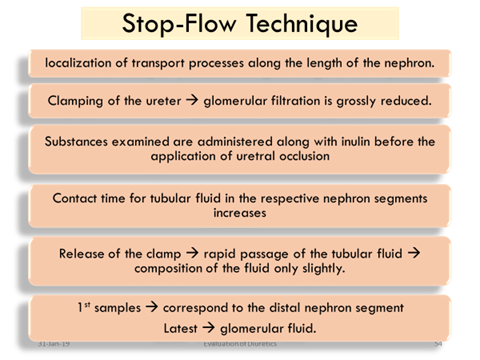
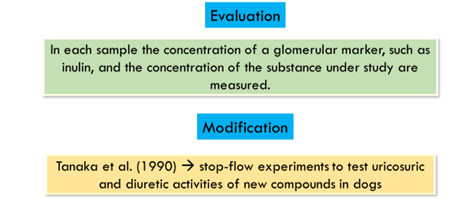
- Segmental nephron studies: To localize the site of action.
- Hydration protocol: Drug/control administered. 20 ml/kg waterload over 20 mins. Voiding is done every 20 min. Blood samples are collected at midpoints of each collection period for clearance calculations. Clearance values and electrolyte values compared between test and control groups.
- Dehydration protocol: Entire protocol is same but AVP and 3% NaCl is administered to volunteers to maintain a urine output of atleast 4 ml/min.
