Nosocomial Infection
Hospitals bring together vulnerable hosts à Subject them to particular risk of infection à Cause of morbidity and mortality à Limits effectiveness, adds greatly to cost.
Hospital-acquired infection (HAI) ( nosocomial infection)
- An infection acquired in hospital by a patient who was admitted for a reason other than that infection . or
- An infection occurring in a patient in a hospital or other health care facility in whom the infection was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility
Impact of HAI
- Add to functional disability and emotional stress
- May lead to disabling conditions that reduce the quality of life
- One of the leading causes of death
- Add to the imbalance between resource allocation
- Significant cause of increased morbidity and mortality in hospitalized patients
- 80% of all hospital deaths are directly or indirectly related to HAIs (Hugheset al., 2005)
- Prevalence varies from 3.8% to 18.6% depending on the population surveyed and the definitions used (Jensen, 2008)
- Economic burden
Factors influencing development of HAI
The microbial agent –
- Resistance to antimicrobial agents
- intrinsic virulence
- amount of infective material.
Patient susceptibility –
- age
- immune status
- underlying disease
- diagnostic and therapeutic interventions
- extremes of life
Environmental factors –
- Crowded conditions within the hospital
- frequent transfers of patients from one unit to another
- concentration of patients highly susceptible to infection in one area
- Bacterial resistance – multidrug resistant strains of bacteria
Source of the infecting organism
- exogenous(equipment)
- another patient ( cross infection )
- hospital staff
- hospital environment
- endogenous
Modes of Spread of Infection
- By Contact: • Staff • Environment (including operation theatre) • Equipment (including blood products)
- Air borne
- Water borne
- Food borne
Infection by contact
From staff:
- Resident (persistent over time and not readily removed by hand washing)
- Transient (recently acquired from another source)
- Important microorganisms are à S. aureus – Klebsiella – Serratia.
- Other less common organisms are à antibiotic resistant enterococci – C. difficile – Corynebacterium diphtheriae – candida albicans – RSV – Rhinoviruses
From the patient’s environment
- Becomes contaminated with bacteria carried by a patient
- Includes – VRE – MRSA – P. aeruginosa – C. difficile
Infection in operating theater
- Most infections arise from the patient’s own flora
- The remainder are acquired mainly from staff in OT
From equipment
Patients with impaired immunity
- Adhesive plaster contaminated with – Rizopus
- Unsterile wooden tongue depressors- Rizopus
- Bed pans and urinals – C. difficile – antibiotic resistant GNB
- Rectal thermometers – salmonellae – enterococci
- Fiberoptic endoscopes – Salmonella – P. aeruginosa – M. tuberculosis – H. pylori – hepatitis B ( rarely )
Infection by inoculation
- Infrequent in developed world – introduction of single-use disposable needles – satisfactory sterilization of surgical instruments
- Risk of infections still persist in situations like
- transmitted by blood transfusion or tissue donation à Risk of transmission of 3 most important agents – hepatitis B, C and HIV
- accidental injury from contaminated sharp instruments
- contaminated blood
- contaminated infusion fluids
- Infection from contaminated infusion fluid
- TPN fluids such as protein hydrolysate with or without dextrose, readily support the growth of organisms, particularly – Klebsiella – Enterobacter – Candida spp.
Ventilator-associated pneumonia
- Mortality rate: 6-14%
- Risk factors include
- Events that increase colonization by potential pathogens
- Those that facilitate aspiration of oropharyngeal contents into the lower respiratory tract –
- Those that reduce host defence mechanisms in the lung and permit overgrowth of aspirated pathogens
Infection associated with indwelling medical devices
- The predominating bacteria are – CoNS, particularly S. epidermidis – S. aureus – Corynebacteria – Propionibacteria – Streptococci – Yeasts and filamentous fungi
- Intravascular cannulae
- Intravascular grafts: àCardiac valve prosthesis
- Joint prosthesis – S. aureus – CoNS – Enterobacteria – Streptococci ( mainly enterococci )
Air-borne spread
Effectiveness of this route depends on
- number of microorganisms present
- degree of dispersal – survival and retention of pathogenicity by the microorganism in the air or environment –
- sizeof the infecting dose – local and general susceptibility of the persons exposed
Tuberculosis
- Air borne spread can occur by transfer of Very few microorganisms
- Only patients with smear positive pulmonary tuberculosis are regarded as constituting an infection risk and require single room isolation
Pneumococcal infection
- Most infection by S pneumoniae is endogenous
- Diagnosed by Gram stain of sputum- advisable to isolate patients for the first 24 h of treatment
- Protection of vulnerable patients with polyvalent vaccine becomes more important as resistance increases
Meningococcal infection
- Uncommon • Isolation for first 48 h of treatment is advisable
- Among staff, only those who have had close contact with the patient need to be offered prophylactic antibiotics
Viral infection • Chicken pox • Measles • Influenza • Respiratory syncitial virus(RSV) • Small round structured viruses(SRSV) – noroviruses
Fungal infection • Dispersal by spores– most filamentous fungi • Only Aspergillus spp. Have been shown to be a significant cause of air borne infection – after cardiac surgery – in immunosuppressed patients •
Infections associated with water
Legionnaires’ disease à Air cooling towers à Source of infection
Infection acquired from food • Salmonella infections- poultry, eggs • Clostridium perfringens– meat • Can be a source of antibiotic-resistant bacteria – P. aeruginosa – Escherichia coli – Klebsiella spp.
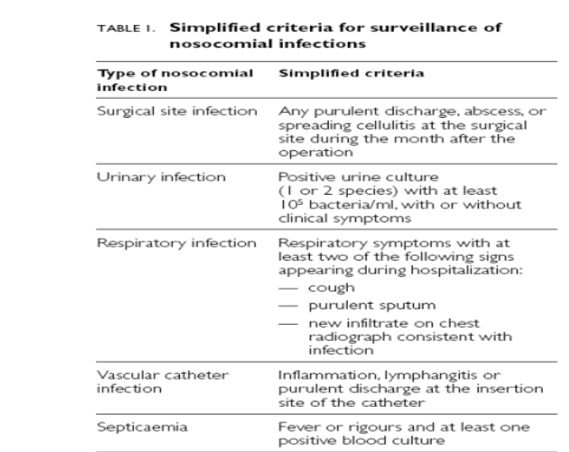
Hospital Infections at various body sites
- Urinary tract
- 40-45% of nosocomial infections
- Associated with – urethral catheterization – cystoscopy – transurethral prostatectomy
- Nosocomial pneumonia
- 15–20% of nosocomial infections
- Almost all cases are caused by aspiration of endogenous or hospital-acquired oropharyngeal (and occasionally gastric) flora
- Early-onset nosocomial pneumonia (within the first 4 days of hospitalization) – Streptococus pneumoniae – Haemophilus species
- Late-onset pneumonias – S. aureus – P. aeruginosa – Enterobacter species – Klebsiella pneumoniae – Acineto bacter
- Surgical site infections
- 0.5-15% of HAI
- A cause of morbidity, prolonged hospital stay
- S.aureus( MRSA )- dominating species
Infection after cataract surgery has declined • Endophthalmitis- following surgery, penetrating trauma • Keratoconjunctivitis caused by P. aeruginosa • Epidemics caused by adenovirustype8 – speed by instruments, hands of staff • Hospital acquired bacterial conjunctivitis-in neonatal units
Peritoneum
- Peritonitis is one of the classical association of surgery
- Peritoneal dialysis is often complicated by peritoneal infection by GNB
Burns
- Suitable site for bacterial multiplication
- S. aureus and P. aeruginosa-most common isolates • Enterobacteria • Other gram negative bacilli such as acinetobacter
Hospital Infections at extremes of life
How are these different…? • Immunocompromised states • Hospital infection and infection control is often neglected – Declining defenses – Multiple underlying chronic diseases – Long stay at hospitals
Neonatal units • Underdeveloped defenses, lack of normal flora (particularly in premature babies) • Ill babies require much handling by staff • CAUTION: – MRSA – Klebsiella – P. aeruginosa – Serratia – S. epidermidis
Hospital acquired infections Management and control
- a well-conducted surveillance and prevention program may significantly reduce HAI and associated costs
- Identification of high-risk population – Burns patients • Immunodeficient patients • Transplant recipients • Chronically debilitated patients • Major surgery • Ventilator support • Indwelling catheters • Prolonged ICU stay (>3 days) • Old age • Frequent blood transfusion
- Isolation • Keep the patient away from potential sources of infection • Assess the need for isolation – Neutropenia and immunological disorder – Burns – Diarrhea – Skin rashes – Known communicable disease – Carriers of an epidemic strain of bacterium • Identify the type of isolation – Protective isolation – Source isolation
- Isolation rooms should have: – Tight-fitting doors – Glass partitions for observation – Negative -pressure (for source isolation) ventilation – Positive- pressure (for protective isolation) ventilation
- Identification of diseases at an early stage
- Treatment
- Periodic surveillance
- Observing hand hygiene – Hands are the most common vehicle for transmission of organisms • Single most effective means of preventing the horizontal transmission of infections among hospital patients and health care personnel
- Strategies to reduce VAP, CAUTI à Designated infection control team(s) *VAP: ventilator associated pneumonia *CAUTI: catheter associated urinary tract infection
- Strategies to reduce UTI • Catheters only for appropriate indications • Closed drainage system • Unobstructed urine flow • Changing indwelling catheters at fixed intervals is not recommended • Remove the catheter when it is no longer needed
- Strategies to reduce VAP • Avoid intubation whenever possible • Prefer oral intubations to nasal • Keep head elevated at 30° 45° in the semirecumbent position • Daily oral care with chlorhexidine solution • Routine change of ventilator circuits is not required • Prefer endotracheal tubes with a subglottic suction port • Closed endotracheal suction systems are better • Periodically drain and discard any condensate
- Strategies to reduce CRBSI • Avoid femoral route for central venous cannulation, prefer upper extrimity • Maximal sterile barrier precautions, and a sterile fullbody drape while inserting CVCs • Clean skin usually with 2% chlorhexidine with 70% ethanol • Chlorhexidine/silver sulfadiazine or minocycline / rifampin impregnated CVCs • Ultrasound guided insertion • 2% chlorhexidine wash daily for skin cleansing
Environmental factors
- High quality cleaning and disinfection of all patient care areas, bedrails, bedside tables, doorknobs and equipment
- Surface cleaning (walls) twice weekly, floor cleaning 23 times/day and terminal cleaning (patient bed area) after discharge or death
- Situated close to the operating theater and emergency department for easy accessibility, but should be away from the main ward areas
- Central air conditioning systems with appropriate filters, air should be filtered to 99% efficiency down to 5 μm
- Isolation facility should be with both negative and positive pressure ventilations
- Adequate space around beds is ideally 2.53 m
- Adequate number of washbasins with alcohol gel dispensers
Organisational and administrative measures • Better patient to nurse ratio in the ICU • Controlling traffic flow to and from the unit to reduce sources of contamination • Waste and sharp disposal policy • Education and training for ICU staff • ICU protocols and SOPs • Audit and surveillance of infections and infection control practices • Infection control team (multidisciplinary approach) • Antibiotic stewardship • Vaccination of health care personnel
Infection Prevention in Burns Patients • Burn wounds can provide optimal conditions for colonization, infection and transmission of pathogens • Source of infection: staphylococcistaphylococci located deep within sweat glands and hair follicles • Routine surveillance cultures: – Early identification of organisms – Monitor the effectiveness of current wound treatment – Guide an appropriate antibiotic therapy – Weekly • Stringent isolation guidelines • Antibiotic prophylaxis: role of topical antimicrobials > systemic antibiotics
Early enteral feeding: increases circulation to the bowel, thereby decreasing ischemia post injury and the translocation of bowel flora • Human tetanus immunoglobulin (250500 IU)
Immunocompromised and Transplant Patients • Greatest risk of infection caused by airborne or waterborne microorganisms • Neutropenic for prolonged periods (ANC < 500 cell/cumm) • Opportunistic infections
Opportunistic infections – Exogenous acquisition of a particularly virulent pathogen, e.g. meningococcal meningitis or pneumococcal pneumonia – Reactivation of an endogenous latent organism, eg, herpes zoster virus, Mycobacterium tuberculosis – Endogenous invasion of a normally commensal or saprophytic organism
Post transplant period 1. During the first month after transplantation: – >95% of the infections are due to bacterial or candida infection of the surgical wound, vascular access, endotracheal tube, or drainage catheters 1. During the period 16 months after transplantation: 1.Two classes of infection : Infections caused by immunomodulatory viruses and infections caused by opportunistic pathogens such as Pneumocystis carinii, Listeria monocytogenes and Aspergillus species • In the late period: 1.Cryptococcus neoformans, P. carinii and L. monocytogenes
76. Monitoring of Infection Control
Antimicrobial Stewardship
- Multidisciplinary antimicrobial stewardship program
- Antibiotic stewardship refers to a set of coordinated strategies to improve the use of antimicrobial medications with the goal of enhancing patient health outcomes, reducing resistance to antibiotics, and decreasing unnecessary costs
- Infectious disease physician and a clinical pharmacist with infectious disease training
- Clinical microbiologist, an information system specialist, an infection control professional and hospital epidemiologist
- Close collaboration between the antimicrobial stewardship team, microbiology lab, hospital pharmacy and infection control team
