Total Parenteral Nutrition
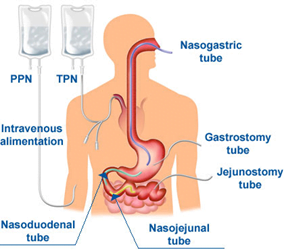
Parenteral Nutrition is pharmacological therapy, where nutrients, vitamins, electrolytes and medications are delivered through venous route, to those patients whose GIT is not functional or unable to tolerate enteral nutrition
Parenteral nutrition is process of supplying nutrients via the intravenous route
- Total parenteral nutrition (TPN)
- Peripheral parenteral nutrition (PPN)
Goals of Parenteral Nutrition
- Maintain or improve nutritional status
- Minimize deleterious effects of catabolism
- Boost immune system
- Improve CVS and respiratory function
- Acid/base and electrolyte balance
- Rehabilitation
Calorie/Protein Yields
- 1 Gm protein = 4 kcals
- 1 Gm fat = 9 kcals
- 1 Gm dextrose = 3.4 kcals
- 1 Gm nitrogen = 6.25gm protein
Peripheral Parenteral Nutrition
- Peripheral vein
- Short period < 2 weeks
- Osmolarity < 900 mOsm/L
- Lipid is an important component
Indications
- Parenteral nutrition for short period
- Central venous catheter insertion not possible
- Sepsis in patient on TPN
Contraindications
- Patients with increased energy requirements
- Patients who are on fluid restrictions
- Critically ill patients who will not tolerate large volume of PPN
Total Parenteral Nutrition
- More effective compared to PPN
- Via Superior venacava or Inferior venacava
- Dextrose used 50-70%, therefore hypertonic and irritant
- Catheter is made of polyurethrane (short period) and silicon rubber (long period)
- It can be Short term TPN or Long Term TPN – “Tunneled”
- System of Delivery :
– Multiple bottle system
– Three in one system - Duration
– Continuous : reserved for critically ill patients
– Cyclic
Indications of Parenteral Nutrition
General Indications
- Inadequate nutrition for least 7-10 days
- Pre-existing severe malnutrition with inadequate oral or enteral feed
Anticipated or actual inadequate oral feeds
- Conditions impairing absorption of nutrients
- Entercutaneous fistula
- Short bowel syndrome
- Effects of radiation and chemotherapy
- Need for bowel rest
- Pancreatitis
- Inflammatory bowel disease
- Ischemic bowel
- Peritonitis
- Pre and post-operative status
- Motility disorders
- Inability to achieve or maintain enteral access
- Significant multi organ failure
Nutrition requirements
Resting Energy Expenditure
Simple body weight formula :
Resting energy expenditure (REE) {kcal/day}=25 × Wt(kgs)
Harris Benedict equation
- REE(men)= 66+(13.7× Wt) + (5 × H(cms)) – (6.7×A(yrs))
- REE(women)= 655+(9.6× Wt) + (1.8 × H(cms)) – (4.7×A(yrs))
Carbohydtrates
- Mainly Dextrose
- 1gm=3.4Kcal
- Variable concentration : 5-70%
- Osmolarity: 252-1900 mOsm/L
Advantages
- Cost
- Calories
- Nitrogen sparing effect
Disadvantages
- Calories as compared to lipids are low
- Increased CO2 production
- Thrombophlebitis
Fats
- Administered as emulsions
- Soybean and sunflower oil
- Egg yolk phospholipids – emulsifying agent
- Glycerin – Isotonicity with plasma
- 1gm = 9 Kcal
- Available as 10, 20 & 30%
Requirements 20-30% of total REE
Advantages
- Calories
- Glucose and nitrogen sparing
- Less carbon dioxide
- Prevention of EFA deficiency
- Less risk of thrombophlebitis
Contraindications
- Hyperlipidemia TG > 350 mg/dl
- Acidosis pH < 7.3
- Anemia
- Intravascular coagulation
- Impaired circulation
Duration :
- If used to prevent EFA deficiency – 3-4days/week
- If used as calorie source – daily
Proteins
- 1gm = 4 Kcal
- 50% EAA + 50% NEAA – standard preparation
- Concentration range 3 – 15%
Advantages
- Calorie supplement
- Protein synthesis
- Decreases rate of catabolism
Contraindications
- Hepatic insufficiency
- Renal failure
- Metabolic or respiratory alkalosis
Monitor Nitrogen balance = Nitrogen intake – Nitrogen loss
Nitrogen loss = {(24 – urine urea Nitrogen + 4) × 6.25 }
+ve Nitrogen balance = anabolism
-ve Nitrogen balance = catabolism
Disease specific modifications
- Hepatic insufficiency
Branched chain amino acids (BCAA ) = leucine, isoleucine & valine
- Renal Failure
Large amount of Essential amino acids(EAA)
- Volume overload
15% concentrated amino acid solution
Special formulations
Immunomodulators
- Glutamine
- Omega 3 Fatty Acid
- Arginine
- Vitamins
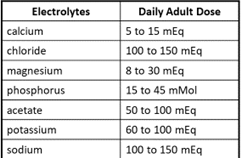
- Electrolytes
- Trace elements
Complications of TPN
- Acid-base imbalance
- Dehydration
- Elevated serum triglycerides
- Failure to induce anabolism
- High serum lipid concentrations
- Hyperammonemia
- Hyperglycemia or hypoglycemia
- Hypoalbuminemia
- Imbalance of electrolytes
- Liver toxicity
- Catheter Sepsis
Designing Parenteral Nutrition formula
3 steps
- Calculation of daily requirements
- Convert requirement into prescription
- To prepare PN solution as per prescription
Step 1
- Fluid requirements = 35ml/Kg
- 35 × Wt(60kgs) = 2100ml
- Calorie = 25 Kcal/kg/day = 25 × 60 = 1500Kcal/day
- Proteins needed for a stable patient is 1gm/kg = 60gms/day
1gm = 4 Kcal
- 60gms = 240 Kcal
- Fats = 30% of energy = 30% of 1500 Kcal = 450 Kcal
- 1gm = 9 Kcal
- Therefore 450 Kcal = 450 / 9 = 50gms
- Carbohydrates = 1500 – (450 + 240) = 810 Kcal
- 1gm Carbohydrate = 4 kcal
- Therefore 810 Kcal = 810 / 4 = 202.5gms
Step 2
Determine volume of lipid emulsion
- Select 10 % emulsion
- Fluid volume (ml) = amount of substance (gms) / concentration (%) × 100
- 50 / 10 × 100 = 500ml
- 500ml of 10% emulsion of fat
Determine volume of proteins (10%)
- Fluid volume (ml) = amount of substance (gms) / concentration (%) × 100
- 60 / 10 × 100 = 600ml
- 600ml of 10% solution of amino acid
Determine concentration and volume of dextrose
- Fluid volume (ml) = amount of substance (gms) / concentration (%) × 100
- 2100 – (500 + 600 ) = 1000ml
- 1000 = 20 / concentration (%) × 100
- Concentration = 20 / 1000 × 100 = 20%
Osmolarity limits
- Peripheral: 600-900 mOsm/L
- Total: > 1800 mOsm/L
Increased osmolarity limits allows for increased concentrations of dextrose and amino acids to be delivered
Osmolarity of additivies (per 1% final concentrations)
- Amino acids: 100 mOsm/L
- Dextrose: 50 mOsm/L
- Lipids: 1.7 mOsm/L
- Electrolytes: 1-1.4 mOsm/meq
Common Additions to TPNs
Precautions
- Phosphates are injected first and are never mixed with calcium and magnessium
- Then add amino acids, dextrose, lipids, and water
- Then add the other electrolytes
- TPN must be inspected after mixing to look for precipitates
Transition to enteral or oral feeds
- Ultimate goal = switch to oral
- Gradual not abrupt
- Once patient can take 60% of total calorie requirements orally, Parenteral Nutrition can be stopped
- Before stopping Parenteral Nutrition infusion rate is decreased to 50% for 2-4hrs
