Antidepressant Drugs
Depression results due to decreased monoaminergic (5-HT and NA) activity in the brain, therefore drugs increasing their activity are called typical anti-depressants.
Drugs acting by other mechanisms are called atypical anti-depressants.
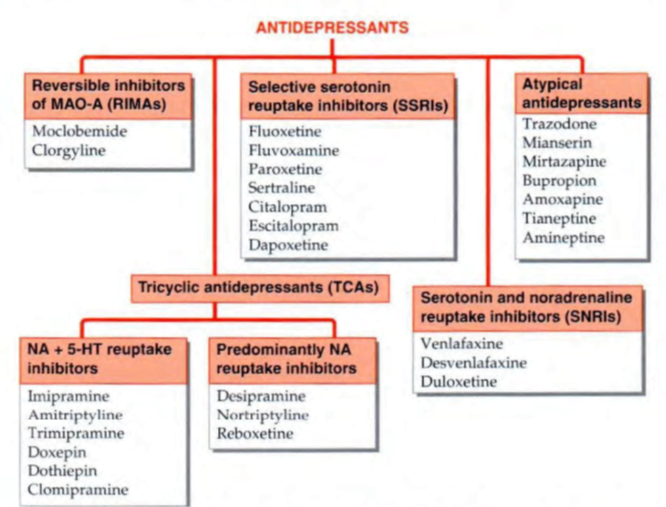
A. Typical Antidepressants
Drugs may increase monoaminergic transmission by inhibiting the reuptake or metabolism of 5-HT or NA.
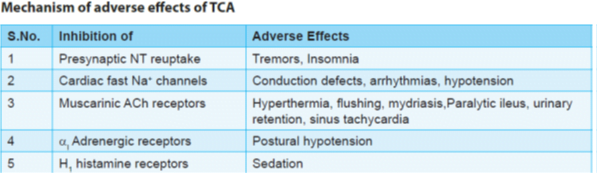
1. Tricyclic Antidepressants (TCA)
- inhibit norepinephrine transporter (NET) and serotonin transporter (SERT) located at neuronal/platelet membrane at low and therapeutically attained concentrations.
- inhibit monoamine reuptake and interact with a variety of receptors viz. muscarinic, α adrenergic, histamine H1, 5-HT1, 5-HT2 and occasionally dopamine D2.
Bupropion (atypical) also inhibits dopamine reuptake. NA and serotonin initially act on presynaptic a2 and 5HT1A receptors respectively and decrease the firing of locus ceruleus (NA) and nucleus raphe magnus (5HT).
- On long term administration, desensitization of these receptors occurs and enhanced transmission is seen.
- This explains the long latency (2-3 weeks) for the anti-depressant action of TCA and SSRIs despite immediate inhibition of reuptake process.
Adverse Effects
• Sedative action of TCAs appears immediately and these drugs (particularly clomipramine, maprotiline and bupropion) lower the seizure threshold.
• Weight gain is another problem with the use of TCAs.
• Most TCAs possess powerful anticholinergic and weak α blocking properties.
Overdose manifestations are mainly anticholinergic (delirium, urinary retention, blurred vision and constipation) in nature.
These also cause postural hypotension (due to α blockade) and cardiac arrythmias at toxic levels.
• TCAs have low safety margin.
• Amoxapine acts by blocking D2 receptors in addition to the inhibition of NA reuptake. It possesses antipsychotic properties as well (It is a metabolite of antipsychotic drug; loxapine). However, risk of extrapyramidal symptoms and convulsions is also present.
• TCAs (impiramine) are also indicated for nocturnal enuresis in children (However, DOC is desmopressin).
Tolerance to the anticholinergic and hypotensive effects of imipramine-like drugs develops gradually, but antidepressant action is sustained.
2. Selective Serotonin Reuptake Inhibitors (SSRI)
- These drugs inhibit the reuptake of 5-HT only (not NA) and lack anticholinergic and α blocking properties.
- SSRIs are now the first-choice drugs for depression, phobias, OCD, PTSD, bulimia, premenstrual tension syndrome and panic attacks because they offer several advantages over TCAs:
• No anticholinergic adverse effects
• No sedation or weight gain
• No propensity to cause seizures or arrhythmias
- They are devoid of α adrenergic blocking action—postural hypotension does not occur, making them
suitable for elderly patients.
SSRIs are preferred for prophylaxis of recurrent depression (should be combined with lithium/valproate)
Metaanalysis of comparative trials has shown no significant difference in efficacy among individual SSRI
Important compounds
• Fluoxetine: It is a prototype SSRI and is longest acting drug in this group. It is metabolized to nor-fluoxetine that retains the anti-depressant activity.
- Because of slower onset of antidepressant effect, it is considered less suitable for patients needing rapid effect
• Fluvoxamine is the shortest acting SSRI.
- specifically recommended for generalized anxiety disorder and OCD, rather than for depression
• Paroxetine, sertraline and citalopram are other SSRIs.
• Escitalopram is most specific SSRI.
• Paroxetine is most teratogenic among SSRIs.
Dapoxetine A SSRI which has been developed and is being promoted for delaying premature ejaculation, a property
Dapoxetine acts rapidly and can be taken 1 hour before sexual intercourse.
Combined with behavioural therapies, it has been found to help many sufferers
Adverse effects
- Prominent side effects are gastrointestinal; all SSRIs frequently produce nausea (due to 5-HT3 receptor stimulation), but tolerance develops over time.
- Loose motions are due to 5-HT uptake blockade in the gut and activation of 5-HT receptors on
- enteric plexus neurones.
- Weight gain is not a problem with SSRIs, but they more commonly interfere with ejaculation or orgasm.
- Coadministration of SSRIs with MAO inhibitors can result in serotonin syndrome. SSRIs can cause akathisia.
- Because SSRIs affect platelet serotonin levels, abnormal bleeding can occur.
- Sertraline and citalopram appear to be safest SSRIs to be used with warfarin.
Serotonin syndrome’ manifesting as agitation, restlessness, rigidity, hyperthermia, delirium, sweating, twitchings followed by convulsions can be precipitated when any serotonergic drug (e.g. MAOIs, tramadol, pethidine) is taken by a patient receiving SSRIs.
3. MAO Inhibitors
Two types of monoamine oxidase enzymes (MAO-A and MAO-B) are involved in the metabolism of monoamines.
• MAO-A predominantly metabolizes NA, 5-HT and DA and is present in the intestine, peripheral nerve endings and liver. à Clorgyline, Moclobemide
• MAO-B preferentially metabolizes dopamine and is present in the brain, platelets and liver.
Non selective MAO inhibitors
Tranylcypromine, isocarboxazid and phenelzine
inhibits both isoforms of MAO irreversibly. à HIT and RUN drugs
Their anti-depressant effect takes 3-4 weeks to develop.
These drugs exhibit a large number of drug and food interactions. The important ones are:
Selective MAO -B inhibitors
Selegiline inhibits only MAO-B and is useful in Parkinsonism. It is available as a transdermal patch for treatment of depression.
• Cheese reaction:
Cheese, beer and red wine, pickled meat and fish contain tyramine (indirectly acting sympathomimetic).
Normally it is metabolized by MAO-A present in the intestine and is not absorbed.
In persons taking non-selective MAO inhibitors, tyramine escapes degradation and can lead to hypertensive crisis. It is known as cheese reaction.
So, cheese etc. should not be given to patients on long term non selective MAO inhibitor therapy.
Phentolamine (alpha blocker) is the drug of choice for cheese reaction.
Prazosin or chlorpromazine are alternatives.
• Non-selective MAO inhibitors increase the risk of seizures if given along with pethidine due to enhanced generation of excitatory metabolite nor-meperidine.
• Serotonin syndrome:
If given along with or just after discontinuation of MAO inhibitors, SSRIs can result in serotonin syndrome.
To avoid this fatal condition, SSRIs should be started at least 14 days after discontinuation of MAO inhibitors.
It allows sufficient time for regeneration of MAO.
Reversible inhibitors of MAO -A (RIMA )
- Moclebemide inhibits MAO-A selectively and reversibly. Because of its reversible and short action,
- it does not exhibit cheese reaction with foods.
- It lacks the anticholinergic, sedative, cognitive, psychomotor and cardiovascular adverse effects of typical TCAs and is safer in overdose.
- Particularly good option in elderly patients and in those with heart disease.
It can be used as an alternative to TCAs for the treatment of depression.
B. Atypical Antidepressants
These drugs may or may not increase monoaminergic levels and possess different antidepressant mechanisms.
• Trazodone
prominent α blocker and weak 5-HT2 antagonist.
It produces sedation, priapism (prolonged and painful erection) and postural hypotensionas adverse effects.
• Mianserin
acts by blocking presynaptic a2 receptors but seizure augmenting and bone marrow depressant actions restrict its use.
• Tianeptin and amineptine acts by enhancing the serotonin reuptake (action opposite to SSRI).
• Venlafaxine, milnacipran, levo-milnacipran and duloxetine inhibit reuptake of serotonin and NA but lack anticholinergic and a blocking properties.
These are also referred to as serotonin and nor-adrenaline reuptake inhibitors (SNRI).
Venlafaxine has faster onset of action. It has minimum drug-drug interactions.
• Mirtazapine:
It inhibits presynaptic a2 receptors and thus increases NA and 5-HT release due to inhibition of auto- and hetero-receptors respectively.
Although it increases serotonin levels in synapse, there is selective activation of 5-HT1 receptors due to antagonistic activity at 5-HT2 and 5-HT3 receptors.
Therefore it is also known as nor-adrenergic and specific serotonergic anti-depressant (NSSA).
It has minimal sexual side effects compared with SSRIs. It commonly causes sedation, weight gain, lipid abnormalities and dizziness.
• Bupropion:
It inhibits the uptake of NA and DA.
It is metabolized to amphetamine like compound and possesses excitatory property.
It is used for smoking cessation as sustained release formulation.
It can precipitate seizures at high dose.
• Nafazodone:
It blocks serotonin reuptake and antagonizes 5-HT2 receptors.
It lacks anticholinergic effects (of TCAs) and agitation (seen with SSRI).
It has very short half life and is hepatotoxic.
• Atomoxetine: It is a selective inhibitor of NA reuptake and is useful for Attention Deficit Hyperkinetic Disorder (efficacy similar to methylphenidate).
• Duloxetine (a mixed NA and 5HT reuptake inhibitor) is also useful in treating chronic neuropathic pain e.g. in diabetic neuropathy and fibromyalgia.
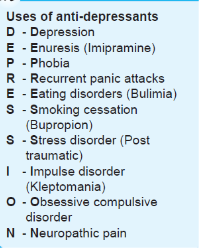
USES
- Endogenous (major) depression:
- The aim is to relieve symptoms of depression and restore normal social behaviour.
- The tricyclic and related antidepressants are of proven value.
- Response takes at least 2–3 weeks to appear, full benefits take still longer.
- Choice of a particular drug for an individual patient depends on the secondary properties (sedative, anticholinergic, hypotensive, cardiotoxic, seizure precipitating, etc.)
- The SSRIs are currently used as first choice for their better tolerability, safety and maybe higher efficacy as well.
- The SNRIs and newer atypical agents also offer some advantages.
- The only antidepressants clearly shown to be effective in juvenile depression are fluoxetine and sertraline.
- The TCAs are mostly used as alternatives in non-responsive cases or in those not tolerating the second generation antidepressants.
- Moclobemide is a well tolerated option for mild to moderate depression, especially suited for elderly and cardiac patients
- Discontinuation of the antidepressant may be attempted after 6–12 months.
- ECT may be given in the severely depressed, especially initially while the effect of antidepressants is developing, because no antidepressant has been clearly demonstrated to act fast enough to prevent suicide.
- The TCAs or SSRIs must be combined with lithium/valproate/lamotrigine for bipolar depression, and not used alone due to risk of switching over to mania.
2. Obsessive-compulsive and phobic states:
- The SSRIs, particularly fluoxamine, are the drugs of choice due to better patient acceptability.
- TCAs, especially clomipramine, are highly effective in OCD and panic disorders: more than 25% improvement occurs in OCD rating scale and panic attacks are reduced in >75% patients.
- SSRIs and TCAs also reduce compulsive eating in bulimia, and help patients with body dysmorphic disorder, compulsive buying and kleptomania, though these habits may not completely die.
3. Anxiety disorders:
- Antidepressants, especially SSRIs, exert a delayed but sustained beneficial effect in many patients of generalized anxiety disorder; may be used along with a short course of BZDs to cover exacerbations.
- SSRIs have also proven helpful in phobic disorders, sustained treatment of panic attacks and in posttraumatic stress disorder.
4. Neuropathic pain:
- Amitriptyline and other TCAs afford considerable relief in diabetic and some other types of chronic pain.
- Amitriptyline reduces intensity of post-herpetic neuralgia in ~50% patients.
- The SSRIs are less effective in these conditions.
- Duloxetine, a SNRI, is now a first line drug for diabetic neuropathy, fibromyalgia, etc. Other drugs useful in neuropathic pain are pregabalin or gabapentin.
5. Attention deficit-hyperactivity disorder (ADHD) in children:
- TCAs with less depressant properties like imipramine, nortriptyline and amoxapine are now first line drugs in this disorder, comparable in efficacy to amphetamine like drugs, with the advantage of less fluctuating action and fewer behavioural side effects.
6. Premature ejaculation:
- Most SSRIs and some TCAs, especially clomipramine have the common property of delaying and in some cases inhibiting ejaculation (this itself can cause sexual distress).
- The primary treatment of premature ejaculation is counselling and behavioural therapy, but this can be supplemented by drugs.
- Dapoxetine is a SSRI which has been specifically introduced for this purpose. It acts rapidly; 60 mg taken 1 hour before intercourse has helped many subjects.
7. Enuresis:
- In children above 5 years, imipramine 25 mg at bedtime is effective, but bed wetting may again start when the drug is stopped.
- Elderly subjects with bed wetting have also benefited.
8. Migraine: Amitriptyline has some prophylactic value, especially in patients with mixed headaches.
9. Pruritus: Some tricyclics have antipruritic action. Topical doxepin has been used to relieve itching in atopic dermatitis, lichen simplex, etc.
