Blood Substitutes
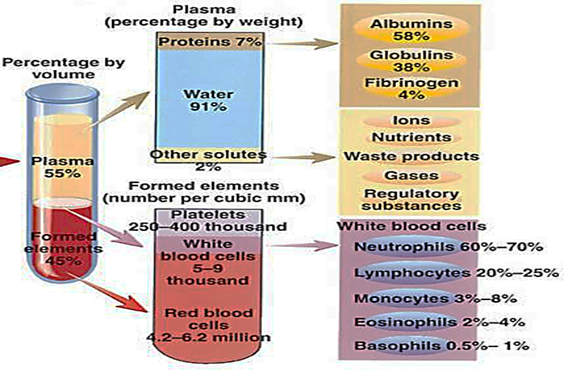
Blood is a special type of connective tissue that is composed of white cells, red cells, platelets, and plasma.
Plasma is the extracellular material made up of water, salts, and various proteins that, along with platelets, encourages blood to clot.
Functions of blood
- Respiration
- Nutrition
- Excretion
- Coagulation
- Maintenance of normal acid base balance in the body
- Regulation of body temperature by the distribution of body heat
- Regulation of water balance through the effects of blood on the exchange of water between the circulating fluid and the tissue fluid
- Defence against infection
- Transport of hormones and regulation of metabolism
- Transport of metabolites
A blood substitute (also called artificial blood or blood surrogates)
- is a substance used to mimic and fulfil some functions of biological blood.
- It aims to provide an alternative to blood transfusion, which is transferring blood or blood-based products from one person into another.
Challenges for blood transfusion:
- Shortage: A very important limitation especially during disasters, wars, emergencies, when it is needed most.
- Short shelf life: This leads to a large amount of wastage of blood.
- Rare blood groups: This can be a problem, especially in under populated areas or in a situation where there is a large demand for blood.
- Immunological incompatibility.
- Disease transmission: HIV, HBV, HCV to name some of the most common pathogens.
Ideal blood substitute
- Oxygen carrying capacity, equalling or surpassing that of biological blood
- Volume expansion
- Universal compatibility: elimination of cross matching
- Pathogen free: elimination of blood contained infections
- Minimal side effects
- Survivability over a wider range of storage temperatures
- Long shelf life
- Cost efficient
Types of blood substitute:
Can serve as
- Plasma volume expanders or
- Replicate the oxygen carrying function of natural blood
1. Plasma Expanders: These are compounds, which are either entirely synthetic or processed from natural proteins that serve as infusion solutions which expand intravascular volume.
2. RBC Substitutes:
Modified Haemoglobins – these are essentially human haemoglobins extracted from outdated blood.
Perflurocarbons – Synthetic organic compounds that can take over perfusion
Plasma Expanders:
Crystalloids:
normal saline, dextrose and ringer lactate.
Can serve as volume substitutes and maintain plasma osmolarity.
Colloid:
plasma expanders encompass a wide range of substances.
These compounds hold water and actually expand volume over the amount infused.
Gelatin:
These are modified gelatin polymers, which were among the earliest used colloid expanders, but are now being phased out due to an inherent risk of anaphylaxis.
Dextran:
This is a newer generation of colloid expander which uniquely not only expands plasma volume, but also serves to decrease blood viscosity, thereby improving perfusion.
Hydroxyethyl Starch (HES):
This is a polymerized form of plant starch which is structurally similar to glycogen and is therefore the safest of the plasma expanders.
Albumins and Purified Protein Derivatives:
These are prepared by fractionating albumin and other proteins from pooled human blood and then sterilizing and processing the albumin so that it is iso-osmolar with plasma. These carry the greatest risk of anaphylaxis.
Uses of plasma expanders
General indications include hypovolemia, loss of blood or plasma or post-surgical states.
- Both crystalloids and colloids have a specific role in overall management of hypovolemia & are life saving products for acute emergency situations requiring resuscitation.
- They are usually used prior to blood transfusion, because no processing or testing of the patient is required for transfusion of expanders and hence can be infused immediately.
Issues with use of plasma expanders
- Anaplylaxis: This remains the chief drawback with plasma expanders. It is particularly prevalent with gelatins and albumins while HES and Dextrans have a very low reported incidence.
- Disease transmission: The incidence of transmission of disease is negligible when compared with blood, but cases have been reported.
- Nephrotoxicity: It is reported especially with dextrans.
- Volume overload and electrolyte imbalance: Can be prevented by careful titration of transfused amount and monitoring.
PFC based blood substitutes
- PFC are biologically inert materials that can dissolve about 50 times more oxygen than blood plasma.
- They are relatively inexpensive to produce and can be made devoid of any biological materials.
- Emulsion particles are 0.2 micron in diameter → Can perfuse smallest capillaries, where no RBC flow.
- Not soluble in water, which means to get them to work they must be combined with emulsions.
- Now a day’s most of the PFBOCs are mixtures of perfluorocarbons with emulsifying agent
- They have the ability to carry much less oxygen than haemoglobin based products.
- This means that significantly more PFC must be used.
- One product of this type has been approved for use by FDA, but it has not been commercially successful because the amount needed to provide a benefit is too high.
Advantages of PFC emulsions
- Do not react with oxygen.
- Inexpensive
- Allow easy transportation of the oxygen to the body.
- They allow increased solubility of oxygen in plasma.
- minimize the effects of factors like pH and temperature in blood circulation.
Disadvantages of perfluorocarbons (PFC) emulsions
- Often causes flu-like symptoms.
- Unable to remain mixed as aqueous solutions – thus, they must be prepared as emulsions for use in patients.
- A decrease in blood platelet count.
- PFC products cannot be used by the human body, and must be discarded.
Examples of PFC based products
| Oxygent | Currently approved for Phase II Trials in US and Europe, developed to ↓ need for donor blood during surgery. Done well overall in most clinical trials, but recently, a cardiac surgery study found participants to be slightly more likely to suffer if treated with Oxygent rather than by standard care. |
| Oxycyte | Currently approved for Phase II-b Trials in the US. Targeted as an oxygen therapeutic, with successful small scale open label human trials treating traumatic brain injury. |
| PHER-O2 | In research |
| Perftoran | Approved in Russian and Mexico. Distributed by KEM Laboratory (Mexico). Its infusion alleviates symptoms of ischemia at different types of occlusion vessels disease, improves grafting in plastic surgery, diminishes inflammation and prevents rejection of transplants, inhibits retro-virus infection development. Local Perftoran applications are able to accelerate wounds and ulcers healing. |
| Fluosol-DA | withdrawn in 1994 due to usage complexity, limited clinical benefit and complications |
Hemoglobin Based Oxygen Carriers
The idea of using purified haemoglobin as a possible universal substitute for red blood cells has been around for nearly a century, based on haemoglobin’s unique oxygenbinding property and the perceived lack of antigenicity. Each normal adult haemoglobin molecule has a tetrameric structure, comprising two alfa and two beta polypeptide chains. Each unit is linked by an iron ion (Fe2+) to a haem molecule, where the oxygen is fixed.
Advantages of HBOC
- Available in much larger quantities.
- Can be stored for long durations.
- Can be administered rapidly without typing or cross matching blood types.
- Can be sterilized via pasteurization.
Disadvantages of HBOC
- Disrupts certain physiological structures, especially the gastrointestinal tract and normal red blood cell haemoglobin.
- They release free radicals into the body.
- Availability and cost.
Nanobiotechnology
Since we can not use free Hb which have several ADRs we should stabilize that Hb with various procedures and then only it can be used.
Nanodimension Complete Artificial RBC.
Concerns
Free radical generation, Iron deposition, Antigenicity
Examples of HBOCs
| Hemopure Polymerised bovine Hb | Currently approved for Phase III trials in US and was more widely approved in South Africa. Many safety measures are taken to render free of pathogens, including herd control and monitoring. |
| Oxyglobin | Currently approved for veterinary use in US & Europe. Oxyglobin solution is the first & only oxygen therapeutic to be both US FDA and European Commission approved for veterinary use. Oxyglobin has been used primarily for blood transfusions and for treatment of anaemia in dogs. |
| PolyHeme Polymerised pyridoxilatedHB | Unique human HBOC in development for the treatment of urgent, large volume blood loss in trauma and surgical settings. It is the only blood substitute that has completed a Phase III trial. Also, free haemoglobin can be taken up by the kidney, causing dysfunction and failure, similar to a hemolytic transfusion reaction |
| Optro Cross-linked HB from genetically modified E. coli | Phase II trials completed. |
| Hemospan Conjugated human Hb | Hemospan is currently in Phase II trials in the US. It is produced in powder form, which can then be mixed into liquid form and transfused immediately, regardless of a patient’s blood type. This technology relies on coupling with polyethylene glycol (PEG) to eliminate the toxicity associated with free haemoglobin. |
| Hemolink Cross-linked human Hb | Phase 3 trials completed. Abandoned due to cardiac toxicity. |
Platelet substitutes
- Infusible platelet membranes
- Red cells with surface-bound fibrinogen
- Liposome-based agents
- Thrombosphere
Blood products grown from stem cells
- RBCs may be grown either from embryonic stem cells or hematopoietic progenitor cells.
- in 2008, Lu et al reported success using embryonic stem cells to grow mature erythrocytes on a large scale.
- However, the cells produced show a phenotype more consistent with fetal or embryonic erythrocytes than adult blood cells.
- Further research will be required to increase yields, eliminate potentially tumorigenic nucleated cells, and determine the half-life and immunogenicity of erythrocytes grown from stem cells.
Other potential techniques
Dendrimers
- Compromises of fluorocarbon and hydrophilic moieties.
- Compatibility with plasma is due to discrete well‐defined globular shapes, flexibility, chemical stability low cytotoxicity and hydrophilicity of exterior makes it a major step forward in the field of blood substitutes e.g. Poly amidoamino dendrimers (PAMAM).
Biodegradable micelles
- To enhance circulation times, recombinant or polymerized haemoglobin can be encapsulated within micellar-forming amphiphilic block copolymers
- The hydrophobic core of polymer micelle is able to solubilize the similarly hydrophobic Hb protein, while the water soluble corona (polyethylene glycol) provides a steric barrier to protein absorption, and provides protection from clearance by RES.
Placental umbilical cord blood
- Cord blood collected aseptically from the placenta after the birth of a healthy baby can be used safely as a blood substitute.
- higher haemoglobin content and growth factors than normal blood from an adult, which has the potential to benefit patients in varying diseases.
Respirocytes
- Are hypothetical, microscopic, artificial red blood cells that can emulate the function of its organic counterpart with increased efficiency.
