- COPD is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.
- Terms emphysema and chronic bronchitis are no more included in the definition.
- Global Prevalence: 11.7%
- Deaths – 3 million annually. Expected to rise to 4.5 million by 2030.
- Second largest non-communicable cause of death in India
- The fourth leading cause of years of life lost in Empowered Action Group (EAG)
- DALYs due to COPD increased 36.3% from 1990 to 2016 and it became the second leading cause of DALYs in India
Pathophysiology
- inflammation of the respiratory tract with a pattern that differs from that of asthma.
- In COPD, there is a predominance of neutrophils, macrophages, cytotoxic T lymphocytes (Tc1 cells), and T helper-17 (Th17) cells.
- The inflammation predominantly affects small airways, resulting in progressive small-airway narrowing and fibrosis (chronic obstructive bronchiolitis) and
- destruction of the lung parenchyma with the destruction of the alveolar walls (emphysema)
- These pathological changes result in airway closure on expiration, leading to air trapping and hyperinflation, particularly on exercise (dynamic hyperinflation).
- This accounts for shortness of breath on exertion and exercises limitations that are characteristic symptoms of COPD.
- Bronchodilators reduce air trapping by dilating peripheral airways and are the mainstay of treatment in COPD.
- In contrast to asthma, the airflow obstruction of COPD tends to be progressive.
- In contrast to asthma, the inflammation in patients with COPD is largely corticosteroid resistant, and there are currently no effective anti-inflammatory treatments.
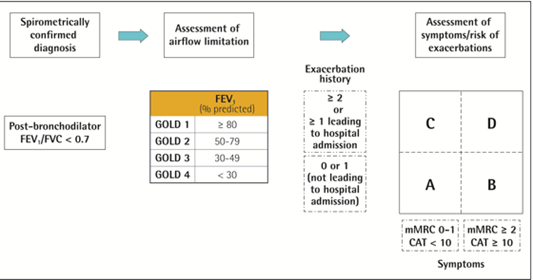
Diagnosis
- Spirometry à post-bronchodilator FEV1/FVC < 0.70 confirms the presence of persistent airflow limitation.
Treatment
Non-pharmacologic Treatment
- Symptom control and palliative care
- Oxygen therapy and ventilatory support
- Surgical interventions
- Vaccination à
- Influenza vaccination can reduce serious illness (such as lower respiratory tract infections requiring hospitalization)24 and death in COPD patients.
- Pneumococcal vaccinations, PCV13, and PPSV23 are recommended for all patients ≥ 65 years of age
Smoking cessation à long-term quit success rates of up to 25% can be achieved.
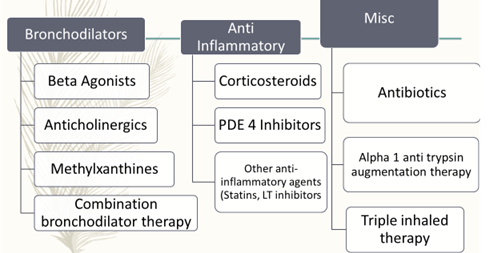
Bronchodilator Therapy
- Inhaled bronchodilators are central to symptom management and given or a regular basis to prevent or reduce symptoms
- Regular and as-needed use of SABA or SAMA improves FEV1 and symptoms.
- Combinations of SABA and SAMA are superior to either medication alone in improving FEV1 and symptoms
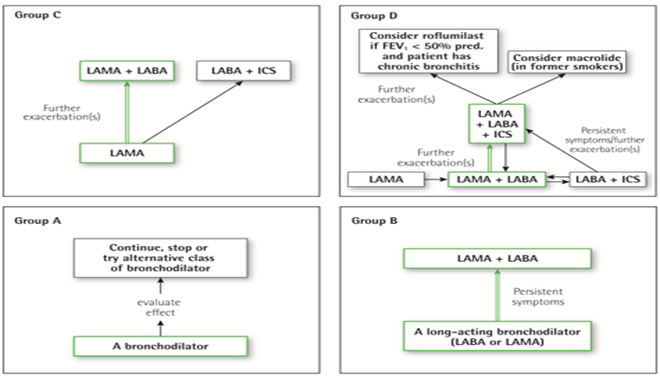
- LABAs and LAMAs significantly improve lung function, dyspnea, health status and reduce exacerbation rates
- LABA + LAMA increases FEV1 and reduces symptoms compared to monotherapy.
- Theophylline exerts a very small bronchodilator effect in stable COPD and that is associated with modest symptomatic benefits.
Anti Inflammatory drugs
- Inhaled
corticosteroids
An ICS + LABA more effective than monotherapy.
Regular treatment with ICS increases the chances of pneumonia. - Triple inhaled therapy of ICS/LAMA/LABA improves lung function, symptoms, and health status.
- Oral
corticosteroids
Long term use of oral glucocorticoids has numerous side effects with no evidence of benefits. - Long term ICS monotherapy is not recommended.
- Longterm ICS + LABA may be considered in patients with a history of exacerbations
- Long term oral corticosteroids not recommended.
- Consider PDE4 inhibitors in patients with exacerbations despite LABA/ICS or LAMA/LABA/ICS
- In former smokers with exacerbations, macrolides can be considered.
- Statin therapy is not recommended for the prevention of exacerbations.
- Antioxidant mucolytics are recommended only in selected patients.
Miscellaneous
- Alpha
1 antitrypsin augmentation therapy
Iv augmentation therapy may slow down the progression of emphysema. - Antitussives
No conclusive benefit - Antibiotics:
Long term azithromycin therapy reduces exacerbations over one year.
It can lead to bacterial resistance and impaired hearing tests.
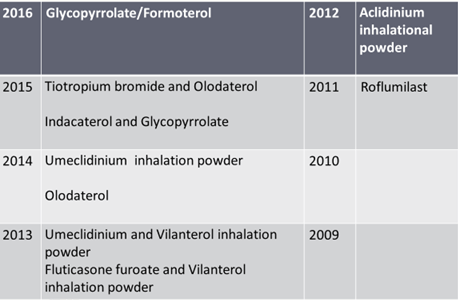
Recently Approved Drugs/ FDCs for COPD
Drugs in pipeline
- Benralizumab
- Mepolizumab
- Lebrikizumab
Asthma-COPD overlap syndrome (ACOS)
asthma-COPD overlap captures the subset of patients with airways disease who have features of both asthma and chronic obstructive pulmonary disease (COPD).
Eosinophilic COPD
- Inhaled corticosteroids + LABA (mixed evidence)
- Anti Ig-E therapies
- Anti IL-5/ IL-5Ra therapies
- Anti IL-13/ IL-4Ra therapies
Neutrophilic Asthma: Macrolides
Pauci-granulocytic ACOS: LAMA
